September 2020 Newsletter
Posted on September 10, 2020.
Welcome to the September 2020 issue of the Global Washington newsletter.
IN THIS ISSUE
Letter from our Executive Director

Every society depends on its children growing up to be healthy, productive, and considerate adults. The UN Convention on the Rights of the Child, ratified just over three decades ago, enshrined the rights that children have, not only to be protected from all forms of violence, but also for the right to realize their potential. It shouldn’t matter where they are born or what gender or circumstances they are born into.
Multiple targets in the Sustainable Development Goals (SDGs) also uphold this commitment to children’s rights. SDG 16 Target 2, for example, sets out to “end abuse, exploitation, trafficking and all forms of violence against and torture of children” by 2030, while SDG 8, Target 7 commits to ending child labor “in all its forms” by 2025.
In this month’s newsletter we examine a rights-based approach to ensuring that children all around the world are able to survive and thrive. You’ll learn how Covenant House is adapting its interventions in response to the COVID-19 pandemic to continue supporting children and youth who have overcome homelessness and trafficking in six countries, including the U.S. Additionally, you’ll meet Mark Dasco, the director of program delivery support for ChildFund International, and this month’s Goalmaker. Mark has spent his career defending and advocating for children’s rights.
If this is a topic you care about, I hope you’ll join me for a virtual event on Friday, Sept. 25 on the alarming increase of child labor and other rights abuses during the ongoing pandemic. I’ll be joined by senior leaders of ChildFund International, Human Rights Watch, and Amplio.
Kristen Dailey
Executive Director
Back to Top
Issue Brief
How a Rights-Based Approach Protects Children During COVID-19
By Joanne Lu

Photo credit: ChildFund International.
Children may be at lower risk of death or severe illness from COVID-19. Nevertheless, the pandemic is threatening to reverse decades of progress made in protecting their rights globally. Because of the socio-economic fallout of the pandemic, billions of children are now at high risk of being forced into the labor market, as well as experiencing sexual exploitation, teenage pregnancy, early marriage, and domestic violence, and falling behind or dropping out of school.
Last year, the world celebrated 30 years since the United Nations (UN) General Assembly adopted the Convention on the Rights of the Child – “the most rapidly and widely ratified international human rights treaty in history,” according to the UN. The treaty, which emphasized children’s rights to survival, development to their full potential, and protection against abuse, neglect and exploitation, paved the way for children to be recognized as “human beings with a distinct set of rights, instead of as passive objects of care and charity.” Although the U.S. has never ratified the treaty – and, in fact, is the only country not to do so – the UN says that the “unprecedented acceptance of the Convention clearly shows a wide global commitment to advancing children’s rights.”
That global commitment is also reflected in the Sustainable Development Goals (SDG), particularly SDG 16 Target 2, which aims to “end abuse, exploitation, trafficking and all forms of violence against and torture of children” by 2030. SDG 8 Target 7 also set a goal to end child labor “in all its forms” by 2025.
Over the last two decades, child labor worldwide has dropped by nearly 40 percent, according to the UN’s International Labour Organization (ILO). Instead of working, tens of millions of children are in school, building better futures for themselves and their communities. And just last month, “the world reached an important milestone…in the fight to end child labor,” as Human Rights Watch put it, when all 187 member countries of the ILO committed to eliminate hazardous work that endangers children by ratifying ILO Convention No. 182 on the Worst Forms of Child Labor.
Still, even before the pandemic, the ILO estimates 152 million children were engaged in child labor, and according to UNICEF, up to one billion children were subjected to physical, sexual or emotional violence or neglect in the past year. Then, COVID-19 hit, causing the worst global recession in decades and shuttering classrooms for 91 percent of the world’s students.
In times of economic hardship and insecurity – like the widespread job losses brought on by the pandemic, as well as parental illness and death – rates of child labor, trafficking and child marriage are likely to increase. According to Human Rights Watch, children who are out of school are also “far more likely to join the workforce, and the longer they stay out of school, the less likely they are to return.”
In this digital age, many schools have been able to switch to online and home learning, but it has been far from the perfect solution. According to a new report by the UN Children’s Fund (UNICEF), when schools closed because of the pandemic, remote learning wasn’t an option for at least 463 million children, because they didn’t have access to the necessary technology and tools. But the report notes that the situation may have been even worse, because even with access, many children may not be able to learn at home because of competing factors, like chores, being forced to work, a poor environment for learning and a lack of support in navigating online or broadcast schooling.
In July, World Vision published a report, which found that due to “plummeting” household incomes and other “COVID-19 aftershocks,” 8 million children have been pushed into child labor and begging. The report includes a call to action to policymakers and other actors to scale up child-sensitive social protection programs, such as food, cash and voucher assistance, to help families meet immediate food, nutrition and income needs, and thereby reducing children’s exposure to violence, exploitation, begging, early marriage, forced labor and the likelihood that they will drop out of school. World Vision has also rolled out emergency cash programming to reach more than 4.4 people, including 2.2 million children, in more than 35 countries.
In addition to financial assistance, Human Rights Watch says that in order to prevent child labor, it’s also important to support decent employment for adults, ensure free primary and secondary education for children, and find innovative ways, including remote reporting, to monitor child labor.
Times of financial crisis also tend to increase rates of early marriage, as marrying off a daughter means one less mouth to feed, a way to repay debts or, in communities where a groom pays a “bride price” to a girl’s family, a source of income. In communities where a bride’s family pays the groom a dowry, a young, uneducated bride is usually much cheaper. In an effort to prevent child marriages during this crisis, Girl Rising’s partners in Kenya have created networks with community leaders who are keeping tabs on girls within their communities to ensure that the girls are not being married off and can return to schools when they reopen.
The UN has also reported that amid the stress, isolation and confinement of the pandemic, there’s been a global surge in domestic violence, with calls to helplines doubling and tripling in some countries. Combined with financial insecurity, Covenant House International says this trend means they’re expecting an uptick in youth homelessness. The organization, which offers housing and support for homeless, runaway and trafficked youth, has stepped up its services to make sure that vulnerable youth have a safe place to stay, especially because kids facing homelessness are particularly vulnerable to being trafficked.
But the pandemic has also changed the way that kids are being trafficked and exploited. Because kids are spending more time online for school and other activities while they’re home, criminal groups dedicated to sexual exploitation have intensified their use of online communication and exploitation. The European Commission reports that demand for child pornography has increased by up to 30 percent in some EU countries during lockdown. According to ChildFund International, exploiters are luring children to engage in online sexual exploitation and abuse by saying it’s a way for them to help support their family financially. But in many cases, victims’ own caregivers are the ones facilitating the exploitation because of financial insecurity. ChildFund International has been working with policymakers on this problem for years, but to combat the recent wave, the organization is reaching out directly to parents through webinars and celebrity-laden social media campaigns to teach them how to protect their children online.
But for millions of children living in refugee or internally displaced persons camps, or detained in the justice system, immigration detention or other institutions, their vulnerabilities, even to COVID-19 itself and other diseases, are heightened. During this time, the work of Kids In Need of Defense has not slowed, as they continue to advocate for the protection of unaccompanied refugee and immigrant children and provide pro bono legal representation for them.
In many ways, children are the most vulnerable amid this pandemic and its socio-economic fallout. But the solutions don’t have to be complicated, so long as we regard children as whole human beings with all the rights that entails. It’s more important now than ever that the international community continues to monitor issues like child labor, trafficking, early marriage and sexual exploitation and abuse. Additionally, if we provide children and their families with the financial support they need to get through this crisis, as well as safe, innovative ways to stay in school, kids may have the chance to show us they’re even more resilient than we know.
# # #
The following GlobalWA members are working to uphold and defend the rights of children globally.
ChildFund International
Worldwide, 570 million children live in extreme poverty, vulnerable to many factors that threaten their well-being. Children need protection, support and care at each stage of childhood to stay safe, healthy, learning and on track to achieve their potential. ChildFund works with local partner organizations, governments, corporations and individuals to help create the safe environments children need to thrive. As more children are spending unsupervised time online for remote learning and social connection, ChildFund is increasingly focused on prevention and responses to online sexual exploitation and abuse of children. The organization has been training parents on how to protect their children from online predators, as well as working with technology companies, governments, civil society, and the media.
Covenant House International
Covenant House has transformed the lives of more than a million homeless, runaway, and trafficked young people in 31 cities across six countries: the U.S., Canada, Guatemala, Honduras, Mexico, and Nicaragua. Covenant House uses a “continuum of care” model that includes mental health care, substance use treatment and prevention, education and job readiness programs, legal aid services, pre- and post-natal support for young mothers, and transitional and supportive apartment living programs. During the COVID-19 crisis Covenant House has been keeping its sites open 24-7, and repurposed physical space to accommodate sick or symptomatic youth, so even if they test positive, they still have a safe place to stay.
Friends of WPC Nepal
There has been a rise in human trafficking in Nepal, as people are desperate to make ends meet during the pandemic. Friends of WPC Nepal funds a safe home in Hetauda, Nepal, for 28 children who are at-risk or survived trafficking, and sends them to private school. The organization also provides scholarships for 58 children in the Hetauda community, as education combats the risk of trafficking and provides a better future. Friends of WPC Nepal also conducts a Trafficking Awareness and Child Rights program that reaches rural villages in Nepal where trafficking is prevalent. This program educates children and families on how to recognize deceptive promises from traffickers and to report it to community leaders and authorities. This program even led to the takedown of a well-established trafficking network.
Kids in Need of Defense (KIND)
Kids in Need of Defense (KIND) is the leading national organization advocating for the rights of unaccompanied migrant and refugee children in the U.S. In 2008, KIND was founded by the Microsoft Corporation and UNHCR Special Envoy, Angelina Jolie, to address the gap in legal services for unaccompanied minors. Through strategic partnerships, KIND provides pro bono legal representation for refugee and migrant children across the country. Over the past decade, KIND has expanded its services to develop a holistic strategy for addressing the needs of these children and the systemic causes of forced migration. This includes mental and social services, advocating for new law and policy in the U.S. and countries of origin, and educating policymakers and the broader public about these issues. To date, KIND has been referred to more than 20,000 children since 2009, has had over 50,000 training participants on how to represent children alone, and fostered over 644 legal partners.
Girl Rising
Millions of girls around the world are kept out of school, married as children, abused, trafficked and discriminated against. Simply because they are girls. Girl Rising uses the power of storytelling to change the way the world values girls and their education. When girls are valued and educated they become women who are healthier, have fewer children, earn more, stand up for their rights and educate their sons and daughters equally. Families thrive. Communities, nations and the world are healthier, safer, and more prosperous.
Human Rights Watch
Human Rights Watch investigates and reports on abuses happening in all corners of the world and directs its advocacy towards governments, armed groups and businesses, pushing them to change or enforce their laws, policies and practices. After having interviewed students, parents, and teachers in 55 countries about their experiences during the pandemic, Human Rights Watch warns that “[g]irls, children with disabilities, children living in poverty, and others are often at greater risk.” As leaders work towards a safe reopening of in-person schooling, here are five things Human Rights Watch recommends doing right away: First, schools that offer remote learning should reach out to students missing from online classes, try to help them re-engage, and provide remedial education. Second, illegal and arbitrary policies that were already keeping children out of school should be lifted. Third, school buildings must be protected, and fourth, affordable, reliable, and accessible internet service must be secured for all students. Finally, any technology recommended for online learning must protect children’s privacy rights.
Save the Children
Unprecedented in scale, COVID-19 is a global crisis that poses immediate threats to children’s rights to survival, development, learning, protection, and to be heard. Unless mitigated, the pandemic risks undermining progress made on achieving the Sustainable Development Goals and puts an entire generation of children at risk of not fulfilling their potential. From the beginning, Save the Children has been working on the ground to ensure that children are protected. This includes providing learning materials for children out of school, working to protect children from violence, and training and supporting health workers in some of the most challenging places in the world. In September, Save the Children launched Protect a Generation, the largest ever global survey of its kind since the pandemic was declared. Covering 46 countries, with 31,683 parents and caregivers and 13,477 children (11-17 years old) participating, the survey revealed that the pandemic has had an especially devastating impact on the education of children from poorer backgrounds and is widening the gap between rich and poor and boys and girls. Two-thirds of the children had no contact with teachers during lockdown; 93 percent of households that lost over half of their income reported difficulties in accessing health services; and violence at home doubled during school closures.
UNICEF
Children continue to be disproportionately impacted by the COVID-19 pandemic that has disrupted everything that we know is critical for children’s social, physical, mental and emotional development, learning and well-being. As a result of COVID-19, nearly 1.19 billion students in 150 countries have been affected by school closures; 80 million children in at least 68 countries may be at risk of diphtheria, measles and polio due to a decline in immunizations; and 369 million children have missed out on school meals. UNICEF contributes to both outbreak control and mitigation of the collateral impacts of the pandemic, including interruptions to water, sanitation and hygiene (WASH), health, nutrition, education, protection and essential social services for children, women and vulnerable populations. The organization is also striving to ensure children are protected at home and in the transition to online environments. To learn more, visit UNICEF’s page on protecting children’s rights: https://www.unicef.org/topics/childrens-rights
Back to Top
Organization Profile
Covenant House Meets Vulnerability with Care
By Amber Cortes

Ana, a former resident of La Alianza in Guatemala, has successfully reintegrated with her family and is now practicing traditional weaving to earn income. Photo: Covenant House.
Covenant House is one of the oldest and largest charities in America dedicated to helping children and youth overcome homelessness and trafficking. Though its roots are in Catholic social justice teaching, Covenant House serves all young people regardless of their backgrounds, religions, and beliefs.
Its constituency is huge—just last year Covenant House reached almost 74,000 youth in the U.S. and globally. The organization operates in 31 cities across six countries: the U.S., Canada, Guatemala, Honduras, Mexico, and Nicaragua.
And in fact, Covenant House has had an international presence for the past 40 years of its almost 50-year history—its second site was built in 1981 in Guatemala, as a response to the vast number of children left orphaned and homeless there during the civil war.
“We’ve actually been international from the very start,” says Chris Megargee, the Seattle-based Latin American Ambassador for Covenant House International. “And it’s kind of unique in that Covenant House is both a domestic and international NGO—there’s not a lot of organizations that fit that bill.”
Covenant House’s commitment to meeting the immediate, basic needs of youth experiencing homelessness in the U.S. includes both drop-in and residential centers.
“When a kid walks through our doors, we’re providing them food, a shower, clean clothes, medical attention, and a safe place to sleep,” explains Megargee. “But we are far more than just a homeless shelter. There’s a broad suite of programs that extends far beyond those immediate needs.”
These programs are part of what Covenant House calls the “continuum of care” model—an array of services, including mental health care, substance use treatment and prevention, education and job readiness programs, legal aid services, pre- and post-natal support for young mothers, and transitional and supportive apartment living programs. These services are provided on site by multi-disciplinary teams of doctors, lawyers, social workers, teachers, and addiction treatment specialists.
“We have a robust lineup of experts to address those broad needs along that continuum of care,” says Megargee.
Megargee describes the programs and services that Covenant House provides as being “very much trauma-informed,” and meant to operate as a bridge from homelessness to hope.
“Because the young people that we’re serving are coming from significant trauma—the trauma that led them to be on the streets, and then the trauma of their harsh life on the streets.”
When it comes to confronting homelessness abroad, Latin America presents distinct challenges for the organization, in a dramatically different socio-economic and political context—one with high levels of poverty, widespread violence, as well as gangs, trafficking, and migration.
Another big difference between Covenant House’s work in Latin America versus the United States is the average ages of youth. In the U.S., the age range of the youth Covenant House serves is between 18 to 22 years old. But in Latin America, the age range is younger—from 12 to 17 years old.
And most Latin American countries, Megargee points out, lack the kinds of social safety nets that exist in North America, like equivalent foster care systems. In the U.S., Covenant House’s focus is on preparing kids for independent living, while in Latin America, the focus is on family reintegration. This includes working with unaccompanied migrant youth who have either started on the migrant trail on their own and turned back because of the danger, or have been separated from family along the way.
Or even deported back by the U.S. In San Pedro Sula, Honduras, a town that borders Guatemala where deportees are dropped off by the busloads, Covenant House works with youth to return them to safe family members and situations. A family reintegration team then keeps track of their progress for two years afterwards to continue supporting them.

A “Zona Libre de Disriminación” (Discrimination-Free Zone) sign welcomes guest arriving at the main entrance of Casa Alianza Nicaragua—a declaration of commitment to creating a safe and supportive space for LGBTQ youth. Photo: Covenant House.
Covenant House operates as “Casa Alianza” in Nicaragua, Mexico and Honduras, and simply, “La Alianza” in Guatemala.
“We refer to them as our Casas,” explains Megargee.
Every night across all four Casas about 350 youth spend the night. And over the course of the year, the full breadth of Covenant House programs in Latin America reaches almost 8,000 youth.
“One thing that we always highlight with the work of the Casas is the level of literal heroism of the staff there,” says Megargee. “Because they’re often serving youth escaping from dangerous situations—gang threats, violence and trafficking—they’re doing their work in a context that puts them at great personal risk.”
For example, in Guatemala, Covenant House staff are working with youth to prosecute their abusers. They also created safe houses specifically for survivors of human trafficking to reside and heal. La Alianza in Guatemala is the only Covenant House site that serves only girls, most of whom have been victims of trafficking or sexual abuse.
In 2012, in Guatemala, La Alianza played a role in the creation of a new government office at the national level dedicated to fighting human trafficking, and was active in passing a national migratory code with a human rights lens, rather than just a security lens.
“Built into that code is recognizing that the issue of trafficking and the reality of migration go hand in hand,” says Megargee.
Since trafficking is big in border areas and towns along the migrant trail,
Covenant House also created a presence in Coatepeque, Guatemala, where it opened a drop-in center located in a very high-risk transit zone, frequented by traffickers and the unaccompanied migrants that they prey upon.
“It’s part of our way of trying to disrupt that machinery of victimization and abuse that happens in trafficking,” Megargee says, adding that each step forward helps “chip away” at the United Nation’s Sustainable Development Goal 16.2—ending abuse, exploitation, trafficking and all forms of violence against children.
On the advocacy level, Covenant House is busy chipping away as well—making shifts on that systemic level, through public education and prevention programs.
“Covenant House started in 1972 as a drop-in center in New York City,” says Megargee. “And now, we’re a movement.”
On the ground, street outreach teams connect with youth to build trust and get them off the streets. Covenant House staff also work with schools, communities, civic organizations, and government agencies to provide information and training on the risks of homelessness and how to spot signs of trafficking.
Despite some of the differences that cause unique situations in Latin America, like trafficking and migration, Megargee sees a common thread among homeless youth everywhere.
“If we think about the vulnerability of youth who are experiencing homelessness, and youth who are on the migrant trail, it’s a similar kind of vulnerability,” says Megargee.
And this kind of vulnerability has only become heightened in the age of COVID—especially for youth experiencing homelessness. Lack of food, health care, and the rough life of the streets leaves this population more susceptible to the novel coronavirus.
“That’s already their norm. And now the stress and anxiety induced by this pandemic on top of that is just unimaginable,” says Megargee.
In addition, jobs have been lost, college classes cancelled, and with the closure of schools, meal production across all Covenant House sites has gone up significantly.
“We’ve been serving 75% more meals because a lot of youth were getting food at school, or if they did have a job, they eat on the job.” Megargee says.
For Covenant House, a frontline organization responding to the crisis, this has meant keeping its sites open 24-7 throughout the pandemic. The organization has also repurposed physical space to accommodate sick or symptomatic youth—administrative spaces and offices have become wellness rooms or quarantine isolation spaces, so even if youth test positive, they can still stay at the site.
Luckily, out of the 2,000 youth sleeping at Covenant House every night across all the sites, only 75 youth to date have actually tested positive, and zero in Latin America—currently the global epicenter for COVID-19 cases right now.
But as is the case throughout the world, the headway that many NGOs and agencies have been making towards the Global Goals is now in jeopardy.
“And thinking back to the Sustainable Development Goals, it’s been this success story about global poverty, the numbers have been going steadily down,” says Megargee.
“But we’re losing ground now because of the pandemic, and certainly that’s the case in Latin America.”
The rise in poverty and hunger puts youth in dangerous situations where they can be preyed upon by traffickers. In fact, the UN Office on Drugs and Crime reported that the pandemic creates new opportunities to exploit vulnerable, economically disaffected youth.
But Megargee hopes that by recognizing the intersectionality among all 17 of the SDGs, progress can still be made—but only if everybody works together.
“Obviously, when we think about the SDGs, we’re thinking about scale, as well. When you look at that wording—’to end abuse, exploitation, trafficking and all forms of violence against and torture of children’—what you realize is that the root causes need to be addressed.”
Confronting poverty and gender inequity, creating access to economic and educational opportunities, promoting good health and well-being—for any one of them to succeed, Megargee says, all of them need to be lifted up.
“And I think that’s the sentiment shared by my colleagues is that there are amazing agencies and NGOs at work on their respective slices of the SDG pie, if you will.”
“So, I have hope,” he adds. “I know we’ll make progress towards the goal. If not, we’ll just move the goalposts and keep working.”
Back to Top
Goalmaker
Mark Dasco, Director of Program Delivery Support for ChildFund International
By Joanne Lu
 Mark Dasco says that growing up in a poor family in a “far-flung village” in the Philippines taught him first-hand the realities of deprivation, exclusion, and vulnerabilities, but it also showed him just how resilient children and communities can be. But just because they are resilient doesn’t mean they should have to be.
Mark Dasco says that growing up in a poor family in a “far-flung village” in the Philippines taught him first-hand the realities of deprivation, exclusion, and vulnerabilities, but it also showed him just how resilient children and communities can be. But just because they are resilient doesn’t mean they should have to be.
Dasco is now the Director of Program Delivery Support for ChildFund International, and he works with Country Office teams around the world to implement strong core programs that address children’s experiences of deprivation, exclusion and vulnerability. But throughout his decades-long career, he’s remained grounded in his home country, where his career began and where he continues to live.
As a child, Dasco says his parents always pushed him to study, because they saw education as the key to success and getting out of poverty. So when he started his career, he decided to become a high school teacher. He spent three years teaching English literature, world literature, Philippine literature, and world history. But after a couple years, a friend convinced him to apply for a position with a child sponsorship organization. He thought his main responsibility would be translating children’s letters to their sponsors into English. But to his surprise, when he got the job, he was assigned to a remote village to facilitate child-centered community development. There, he helped marginalized families organize and mobilize to promote their rights, demand the basic services they deserved, and participate in and benefit from development programs.
“I realized that this job was still teaching and empowering people, but this time it was beyond the four walls of the classroom,” says Dasco.
Around this time, the UN also signed its landmark Convention on the Rights of the Child, the most widely ratified human rights treaty in history, which guarantees children’s rights to education, healthcare, play, and protection from violence. Dasco describes this as a pivotal moment in his career because he was among the first cadre of staff in the organization he was with at the time to become trained advocates of child rights. This experience was Dasco’s first introduction to rights-driven, community-led development work, where initiatives are not done out of pity for children and their communities, but because it’s their right. And development workers aren’t saviors bringing in solutions, but rather facilitators, helping communities drive their own development. These became values that Dasco has integrated into his approach to and practice of development work throughout his 25-year career.
Dasco first found his way to ChildFund International as a business development consultant in Timor Leste. After a few months, he became a program manager. But three months in, the 2006 East Timor conflict erupted, sparking violence and unrest throughout the country and turning his role into that of an emergency response team leader, including helping to create safe spaces for children to participate in psychosocial activities that provide them a much-needed routine and sense of normalcy.
When he finished his stint in Timor Leste, Dasco returned to the Philippines to work as a regional funding manager in the Asia-Pacific region for another organization. But it wasn’t long before he realized that he missed working closely with communities like he did with ChildFund. In his position, he felt detached from the work and its results. So when he saw another opening at ChildFund, he immediately applied and has been with the organization for nearly 12 years.
Even though in his various director positions, he doesn’t always get to work directly with children, Dasco finds real fulfillment in being able to improve the systems around children, because “development doesn’t always trickle down to children,” he says. Children don’t always directly feel the impact, get to participate in it or benefit from it, so he’s made it his life mission to change that.
For example, he says that at ChildFund, they always incorporate the voices and experiences of children into their programming. In Ecuador, for instance, teens are producing their own radio programs to discuss issues and concerns in the community. And in the Philippines a group of children with disabilities are taking the lead on their own community planning, community-based child protection initiatives, identifying issues and problems that impact them and suggesting solutions. Dasco says ChildFund is careful to always use child-friendly methodologies that are based on children’s capacity and developmental levels, that won’t jeopardize their safety, and that will build up their confidence to become their own advocates.
During the pandemic, much of Dasco and ChildFund’s attention has been on prevention and response to online sexual exploitation and abuse of children (OSEAC), as more children are spending unsupervised time online for remote learning and social connection. ChildFund has been hosting webinars and social media campaigns with technology partners that teach parents how to protect their children from online predators. In the Philippines, ChildFund has launched the #ShutdownOSEC campaign on social media with the country’s leading civil society network, where children urge the government to prioritize OSEAC and take stronger actions to address it. In Mexico, ChildFund established a relationship with the Mexican Center for Electronic Crimes against Minors (CENADEM), the government entity responsible for investigating online sexual exploitation and abuse of children. In Ecuador and Kenya, ChildFund is looking to build on its work through a series of initiatives to address increased risks of OSEAC due to COVID-19. The organization will conduct national assessments to identify gaps in OSEAC policies and knowledge, as well as gain an understanding of its prevalence in each country. Because the nature of OSEAC is continuously evolving, ChildFund plans to advocate for governments globally (including the U.S. government) to begin collecting data on OSEAC and its prevalence. Further, ChildFund has joined with technology companies, international alliances such as WePROTECT Global Alliance, civil society, and the media to address this problem.
Dasco was also recently appointed to the Philippines’ Council for the Welfare of Children Board, where he will continue to raise the issue of online sexual exploitation and abuse and advocate for addressing policy gaps, as well as increase the capacity of law enforcement to respond to it.
Currently, Dasco is also leading a task force that hopes to identify alternative program delivery tools that are “low-touch, high-tech, high impact” and, of course, safe for children. Although this task force is inspired by current limitations on interacting face-to-face with communities during a pandemic, it’s also a way for ChildFund to innovate by leveraging technology and partnerships to expand its reach to more children and families.
Dasco and the ChildFund team are looking forward to developing their new global strategy for the next 10 years. “We’re calling it our big, hairy and audacious goal,” Dasco says with a smile. “We’d like to reach 100 million children by 2030.”
Back to Top
From Our Blog
“Years don’t wait for them”: 5 Things to Do Now to Protect Children’s Rights During Covid-19
By Zama Neff
“It does not make me happy that my children are no longer going to school,” the mother of two preschool-age children in North Kivu, a conflict-affected region in the Democratic Republic of Congo, told us. “Years don’t wait for them. They have already lost a lot. . . . What will become of our uneducated children?”
Children around the world face an unprecedented threat to their human rights. Pandemic-related school closures have affected 1.5 billion students, placing children at immediate risk of labor exploitation, hunger, recruitment into armed groups, and, especially for girls, child marriage, and sexual violence. Two decades of gains in reducing child labor and increasing school enrollment are under threat. Read more.
Back to Top
Welcome New Members
Please welcome our newest Global Washington members. Take a moment to familiarize yourself with their work and consider opportunities for support and collaboration!
Child Foundation
Child Foundation is an international charity organization that helps children living in poverty remain in school. The children sponsored through Child Foundation programs are high achievers, and many of them are orphans or children living in emergency situations. By enhancing the quality of life for children in need, as well as their respective families, Child Foundation actively helps them gain access to education. https://www.childfoundation.org/
CORE Group
CORE is the only player in its field that convenes the practitioners and public health professionals in global community health to share knowledge, evidence, and best practices, and then translates these into the real world with a direct impact, creating new standards in clinical and public health as it advances dialogue at the country and global levels. https://coregroup.org/
GAPPS – Global alliance to prevent prematurity and stillbirth
GAPPS seeks to improve birth outcomes worldwide by reducing the burden of premature birth and stillbirths. GAPPS is working to close the knowledge gap in understanding the causes of preterm birth and stillbirth and collaborating to implement evidence-based interventions to improve birth outcomes. https://www.gapps.org/
Save the Children
Save the Children believes every child deserves a future. Since its founding more than 100 years ago, the organization has changed the lives of more than 1 billion children. In the United States and around the world, Save the Children gives children a healthy start in life, the opportunity to learn and protection from harm. The organization does whatever it takes for children – every day and in times of crisis – transforming their lives and the future we share. https://www.savethechildren.org/
Back to Top
Member Events
September 12: Friends of WPC Nepal – Hope For Freedom Gala 2020
September 18: Spreeha’s Journey of Hope – Virtual Fundraiser
October 19: PeaceTrees Vietnam: Celebrating 25 Years of Friendship in Vietnam
Back to Top
Career Center
Bilingual Receptionist // Northwest Immigrant Rights Project (NWIRP)
Marketing and Communications Manager // Splash
Check out the GlobalWA Job Board for the latest openings.
Back to Top
GlobalWA Events
September 16: Final Mile Event: Kicking off a US chapter of the International Association of Professional Health Logisticians (IAPHL) and the COVID-19 work of Restart Partners
September 25: Child Labor Increasing Amid COVID-19 Pandemic
Back to Top
“Years don’t wait for them”: 5 Things to Do Now to Protect Children’s Rights During Covid-19
Posted on September 4, 2020.
By Zama Neff

Children in a favela in Rio de Janeiro watch as a volunteer disinfects public areas during the Covid-19 pandemic, Brazil, April 20, 2020. © 2020 by Mauro Pimental/AFP via Getty Images
“It does not make me happy that my children are no longer going to school,” the mother of two preschool-age children in North Kivu, a conflict-affected region in the Democratic Republic of Congo, told us. “Years don’t wait for them. They have already lost a lot. . . . What will become of our uneducated children?”
Children around the world face an unprecedented threat to their human rights. Pandemic-related school closures have affected 1.5 billion students, placing children at immediate risk of labor exploitation, hunger, recruitment into armed groups, and, especially for girls, child marriage, and sexual violence. Two decades of gains in reducing child labor and increasing school enrollment are under threat.
Continue Reading
PRESS RELEASE: Americares Responds to COVID-19 Surge in Peru
Posted on September 2, 2020.

Patients receive medical care, including COVID-19 testing, at an Americares and VIDA Perú mobile clinic in Lima, Peru, on Aug. 29. Photo by Angela Ponce/Americares.
Stamford, Conn. – Sept. 2, 2020 – Americares is providing surge medical support in Peruvian health facilities overwhelmed by the COVID-19 pandemic. The health-focused relief and development organization is dispatching medical personnel, all of which are locally based and have experience working within the health system, to health centers in Lambayeque, Lima and Piura to meet the increase in demand for care and provide the struggling health system with some relief as the coronavirus pushes health center capacity to the brink.
“As COVID-19 cases rise in Peru and health facilities continue to struggle with an unprecedented demand for services, our medical personnel will provide critically needed manpower,” said Americares Vice President of Emergency Programs Kate Dischino. “Our support will help ensure hospitals and clinics can continue treating patients and access the supplies needed to keep health workers safe.”
Continue Reading
PRESS RELEASE: Mercy Corps Names Tjada D’Oyen McKenna Chief Executive Officer
Posted on August 24, 2020.
McKenna brings proven leadership in humanitarian relief and international development
PORTLAND, OR — The Board of Directors of Mercy Corps today named Tjada D’Oyen McKenna as the global organization’s Chief Executive Officer. McKenna will assume leadership at Mercy Corps on October 15, 2020.
“Mercy Corps is rightly recognized around the globe for innovative, bold responses to the world’s toughest challenges,” says McKenna. “It’s an honor to join this organization and in particular this remarkable global team of nearly 6,000 innovative leaders.”
Continue Reading
August 2020 Newsletter
Posted on August 13, 2020.
Welcome to the August 2020 issue of the Global Washington newsletter.
IN THIS ISSUE
Letter from our Executive Director
 I have two children in Seattle Public Schools, so like many families across the U.S., I am filled with mixed emotions about online learning, rather than in-person classrooms. However, I am grateful that we have an online option and that the school district is working to donate computers to students who need them. For most children in low- and middle-income countries, online learning via computer is not a viable solution. Fortunately, several Global Washington members are working with local governments and schools to come up with creative alternatives, such as delivering educational curriculum to cell phones, as well as using radio and TV broadcasting.
I have two children in Seattle Public Schools, so like many families across the U.S., I am filled with mixed emotions about online learning, rather than in-person classrooms. However, I am grateful that we have an online option and that the school district is working to donate computers to students who need them. For most children in low- and middle-income countries, online learning via computer is not a viable solution. Fortunately, several Global Washington members are working with local governments and schools to come up with creative alternatives, such as delivering educational curriculum to cell phones, as well as using radio and TV broadcasting.
As a parent, I also know that schools provide so much more than just education for children. Again, several Global Washington members are shifting their operations to address the immediate needs of the COVID-19 crisis and are delivering care packages to students’ homes, including feminine hygiene products, soap, and protective masks. Members are also reaching out to female students in particular to assess their safety because reports have shown an increase in domestic violence during the pandemic.
Education is a foundational element of many of the Sustainable Development Goals (SDGs), including economic development, gender equity, and global health. I’m inspired by Global Washington members who have stepped up to this current challenge, ensuring that COVID-19 does not erase all the progress we’ve made in supporting education in developing countries.
In this month’s newsletter, you can read more about this issue. You’ll learn how Pilgrim Africa is keeping students in Uganda safe and making sure they have what they need to continue learning at home. You will also meet an inspiring Goalmaker, Judithe Registre, who is the VP of Programs at Girl Rising, and a firm believer in the power of stories to shape the future. Please also join me on August 21 for an online conversation with Girl Rising, Rwanda Girls Initiative, and Sahar.
Kristen Dailey
Executive Director
Back to Top
Issue Brief
Educators Experiment with Online and Offline Solutions to Distance Learning Around the World
By Joanne Lu
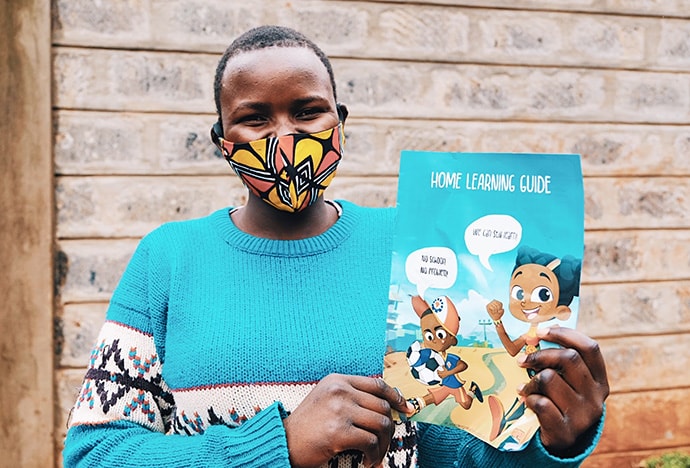
Even with schools closed around the world, learning continues. Girl Rising partner Metis Collective developed a Home Learning Guide, which is being put to good use in Kenya. Photo by Metis Collective.
COVID-19 has caused the biggest disruption in history to education systems around the world, according to the UN. Globally, 94 percent of students have been impacted by school closures – 99 percent in low- and lower-middle income countries – and experts are warning that global education has been pushed back to levels not seen since the 1980s.
Although the start of the school year is upon us, many countries, districts and institutions are still grappling with the best way to re-open schools amid a global pandemic. It is simultaneously critical that schools do their part to suppress transmission of the virus and continue to provide an education, which is not only a fundamental human right but also a key driver of long-term progress for every country. Educated youth are every country’s future potential for growth, and without them, it is impossible to achieve any of the Sustainable Development Goals.
Right now, the UN estimates that 23.8 million children and youth may drop out or not have access to school next year because of the pandemic’s economic impact. Additionally, for many children around the world, school is where they receive their most nutritious daily meal. School closures have also affected the ability of many parents to work and has increased the risk of violence at home, particularly for women and girls.
Amid this historic disruption, many experts, policy makers, schools, organizations and companies are turning to tech and digital solutions to ensure the pandemic doesn’t cause us to fall too far behind. Some institutions, like Northeastern University Seattle have gone completely virtual since March, offering only online classes. Others, like Seattle Pacific University and Seattle University, are adopting a hybrid format, with online and limited in-person classes so that students can benefit from both formats.
Globally, ministries of education and organizations are rolling out online curricula to keep children, particularly those in low- and lower-middle income countries, from dropping out. The pandemic’s impact on poverty means that dropping-out now may result in millions of children never returning to school, according to Save the Children. ChildFund International’s $56 million plan to help 6.3 million children and their family members remain healthy, educated and safe during the pandemic includes online tutoring sessions and activities. The organization is also staying “vigilant and prepared” to address the increased risk of online sexual abuse as more kids are exposed to the internet.
However, especially in low- and lower-income countries, not everyone has access to devices, the internet or even electricity. In India, for example, Girl Rising reports that only 11 percent of all Indians own a computer, and only 8 percent of all households have both a computer and an internet connection. This means that the existing digital divide – the gap between those who have access to computers and the internet, and those who don’t – could exacerbate education inequalities, as only students with more resources are able to keep up with their studies, while the rest fall further behind or drop out. That’s why ChildFund International is also offering activities and lessons by radio and distributing home-learning kits with materials and guidelines for how to use them.
It’s also important to note that the digital divide – and the pandemic’s impact on education as a whole – disproportionately affects women and girls. According to a 2018 report by the Organization for Economic Co-operation and Development, 327 million fewer women than men worldwide have a smartphone and can access the mobile internet. In addition, for girls in many countries, school is where they are safe from violence, where they have access to menstrual hygiene products and a where they can create a future for themselves that lowers their chances of becoming victims of child marriage and adolescent pregnancy. A UN study found that in Sierra Leone, teenage pregnancy increased by 65 percent during the Ebola crisis, as girls were forced to stay out of school and became more vulnerable to sexual exploitation, assault and rape.
Girl Rising works with local partners around the world to provide curricula and tools that empower girls and change attitudes and social norms regarding gender in entire communities. While schools are closed, the organization and its partners are continuing their messaging and education through various means, as well as providing essential supplies like food and sanitary towels. In Guatemala, for example, they’ve adapted the Girl Rising curriculum online, but girls are also helping to produce radio programs to share what they’re going through during this time. Girl Rising’s Kenya partner, Sunflower Global, has developed and is distributing monthly and weekly at-home learning packets to keep students on track with their studies. Meanwhile, in India, Girl Rising is partnering with five state governments to create art curricula for social and emotional learning that can be delivered over basic cell phones.
While so much learning has been moved online, to radio and to mobile formats, it’s still important to make sure that when schools reopen, there are good schools for children to attend. That’s why buildOn has continued to build schools in communities around the world. They’ve reduced the number of community members on worksites to allow for appropriate social distancing, but the work continues.
The UN also says it’s essential to continue investing in teachers as they navigate the changing landscape of education during this time. Pilgrim Africa, which runs a boarding school called Beacon of Hope in Uganda, has managed to pay its teachers their full salaries while the school has been closed. In turn, the teachers are continuing to check on the wellbeing of their students, especially the girls, at home and are providing books and other learning materials. Beacon of Hope has also managed to provide its older students with tablets and online learning tools so that they’ll still be able to take their qualifying exams for university.
Closing the digital divide could not only leave fewer students behind during this pandemic, but it could also create new opportunities for education and work moving forward. For example, in June, Microsoft launched an initiative that will equip 25 million people around the world with the digital skills they need to work in a COVID-19 economy, as well as in an increasingly digital world.
According to a UN report, if all countries in a human development group (low, medium, high or very high development) are able to have the same internet access rate as the top country in their respective group, the rate of out-of-school students this year would drop from 20 percent to 12 percent. And, closing the gap in internet access for low- and middle-income countries wouldn’t be expensive at all: It would only cost 1 percent of the amount of money the world has committed so far to respond to the pandemic. Not only would it increase student’s access to online learning, but it would also allow more people to work from home and access tele-health services.
Until the digital divide is closed, technology and digital solutions cannot be the world’s sole response to education during a global pandemic. But as long as we continue to find ways to reach kids who don’t have access to online learning and simultaneously work to close the digital divide, the world could come out the other side of this crisis with more equitable access to education and a more resilient economy.
# # #
The following Global Washington members are finding creative ways to continue supporting education during the COVID-19 pandemic.
Ashesi University Foundation
Ashesi University remains committed to educating a new generation of ethical and entrepreneurial leaders in Africa. As a result of the COVID-19 pandemic, Ashesi successfully navigated a temporary campus closure and transition to online learning. Accounting for students’ diverse needs, Ashesi has provided travel support to international and local students; stipends for unexpected student costs; data packages in partnership with telecom partners; laptop acquisition and delivery; resources for online learning; and counseling for individual students. Starting August 31st the first semester of the 2020/2021 academic year will operate entirely online and all university activities will be conducted remotely. The connections and experiences shared at Ashesi will not be easily replicated online, but the university is excited about the chance to strengthen the spirit of innovative action that defines it and to pursue ideas that may have seemed far away in the past. The decisions made now have the potential to redefine the Ashesi experience and will impact many generations of students to come. Read more about the Ashesi community response to COVID-19 and learn about the university’s current funding priorities.
ChildFund
ChildFund works in 24 countries throughout Asia, Africa and the Americas – including the United States – to create connections that drive lasting, positive change for children wherever they are. Its programs address the underlying conditions that prevent any child from achieving their full potential. In the Americas, ChildFund has been focused on making sure young people have an opportunity to continue their educations during the COVID-19 pandemic. The organization has produced guides on educational and recreational activities for home use, developed trainings for parents and teachers, hosted virtual training sessions, and developed radio shows with educational content. ChildFund is also supporting schools’ capacity to prevent the spread of the virus. In addition, ChildFund is providing cash-based aid, food, hygiene, and recreation kits to families with young children.
Girl Rising
Girl Rising envisions a world in which girls thrive with dignity and vast possibilities. The organization’s mission is to advance the rights of girls and promote gender equality around the world. At the heart of its work are stories. Girl Rising staff include filmmakers, journalists and international development professionals who have seen the power of stories to transform attitudes, beliefs, and behaviors. They want girls everywhere to be able to go to school, stay in school and have a future of their own choosing. As the world collectively faces COVID-19, the future of millions of girls and their education is uncertain. With in-person learning curtailed, the organization and its partners are distributing educational materials and sharing stories through alternative channels, including cell phones, radio programs, and at-home learning guides.
buildOn
For more than two decades, buildOn has mobilized rural communities to build schools in some of the poorest countries on earth. With the ongoing COVID-19 pandemic, buildOn has continued construction of schools, though the number of community members on worksites has been reduced to enable sufficient physical distancing. To date, buildOn has built 1,323 schools.
Fanikia Foundation
By supporting the cost of boarding at public schools, Fanikia Foundation ensures that disadvantaged girls have access to quality education in rural Tanzania. As in much of the world, schools across Tanzania were closed due to COVID-19, and most students, especially in rural areas, were unable to access remote schooling due to the lack of equipment for both teachers and students. For almost fourteen weeks students in Tanzania missed school at the beginning of the year. As a result, they will need to stay in school longer to compensate for the time they missed. The students that Fanikia supports are now back at their boarding schools and continuing their studies. The global pandemic has caused food to become scarce in parts of Tanzania, especially in rural areas, which in turn has led to an increase in food prices. Fanikia hopes that the situation will not negatively affect the girls’ studies.
Global Visionaries
In Guatemala, the first case of COVID-19 was detected on March 13. Youth in Guatemala were already struggling to access education due to various limitations and a lack of structure in the educational system; the pandemic further aggravated these challenges once the government closed the schools as part of the emergency response. Global Visionaries understands and prioritizes people-centered and inclusive educational programs, and considers them essential for engaging young leaders to create a just, sustainable, democratic and peaceful society. Global Visionaries’ youth education and leadership program continues to engage Guatemalan youth through the Zoom platform, with internet accessibility provided to students in need. The program focuses on recovering historical memory (because traditional education in Guatemala does not adequately address the true history), as well as learning about planet earth, analyzing current government decisions, and understanding how to use one’s voice to make positive changes in society. Global Visionaries has also made space for students to be in community (online) with each other and explore their own frustrations and hardships brought on during this difficult time of isolation. Additionally, staff have been connecting with students individually to address their needs or concerns, such as home safety concerns and mental health.
Human Rights Watch
Human Rights Watch works around the clock to protect the rights of people who face the greatest risks during the Covid-19 pandemic, particularly children. More than 1.5 billion students are out of school, and widespread job losses and economic insecurity will likely lead to increased rates of child labor, sexual exploitation, abuse, and child marriage. Building on its deep expertise documenting and campaigning for access to education for all children, Human Rights Watch is working to ensure that distance education is provided for all children, with special efforts to reach girls, children with disabilities, and others less likely to access current programs. Human Rights Watch is pressing for greater protections for children’s data and privacy online and expanding access to the internet. And it is urging governments to support children in returning to schools when they re-open, reaching out especially to children forced into hazardous work, child marriage, early pregnancy, or who were displaced.
Manos Unidas International
Manos Unidas International provides professional development training, program support, and financial support for organizations serving children and youth in Latin America. In Peru, the government closed all schools due to the COVID-19 pandemic. Manos Unidas has shifted to a virtual environment for its students and families – currently offered free of charge due to economic hardships in the Cusco community. Manos Unidas teachers designed online lesson plans according to the needs of each student group and the available technology – from Zoom to WhatsApp video calls to Google Meet. Each teacher works with 6-8 students, ranging in ages from 4-20 years old. For example, the early childhood autism classroom receives three individual phone calls a week for 30 minutes, and the teacher follows a sequence of learning materials with the families. She instructs the families on how to implement and teach the skill then does a follow-up call two days later. Manos Unidas teachers are also focused on teaching functional skills for independence, such as chores around the house. Older youth are meeting as a group and have been working on pre-recorded classroom sessions. The virtual program will continue on a weekly basis into next year. In addition, a pre-recorded virtual education library will be set up for teachers to share resources.
Mona Foundation
The COVID-19 pandemic has indiscriminately impacted our entire planet and has changed the way we live, work and play. To that is now added a global cry for elimination of systemic racism, and renewed calls for equal justice under law. The pandemic has also brought to light the universal truth that what impacts one, impacts all, and that education is the key driver to eradicating poverty, prejudice, violence and other social ills that afflict our communities, including this disease. But for education to be transformative, it needs to be transformed – teaching lessons of equality, ethics and service alongside math, sciences, and humanities. The field experience of the Mona Foundation’s 19 partner projects in 12 countries in the past few months has confirmed yet again that this view of education is the key lever in creating and sustaining positive change and building healthy, prosperous and just communities for all. The scope of their current activities is considerable and complex. Every partner has transitioned its educational programs online, while also saving lives – providing COVID-19 prevention kits (masks and soap), delivering food, and preventing violence against women. Read the Mona Foundation blog for more information.
Pilgrim Africa
Pilgrim Africa’s mission is to challenge despair, love boldly, and help African people create a future of prosperity and health. In 2005 the organization founded a rural boarding school in Uganda, called Beacon of Hope, for former child soldiers and other children recovering from war. It became one of the first schools outside of the country’s capital, Kampala, to focus on STEAM education: science, technology, engineering, arts, and math. In 2014, the last child soldiers graduated, but the school has continued to open its doors to rural students who would otherwise not have access to high quality education. During the COVID-19 pandemic, Beacon of Hope has managed to pay its teachers their full salaries, even while the school has been closed. In turn, the teachers check in on their students at home, and provide books and other learning materials so that they can continue their studies. The school is also providing older students with tablets and online learning tools so that they will be prepared for their qualifying exams for university.
Rwanda Girls Initiative
Rwanda Girls Initiative’s mission is to educate and empower girls in Rwanda to reach their highest potential. The organization strives to cultivate inspired leaders with a love of learning and a sense of economic empowerment to strengthen their communities and foster Rwanda’s growth. The Gashora Girls Academy of Science and Technology (GGAST) was opened in 2011 as an innovative and socio-economically diverse model upper-secondary school, designed to provide a “whole girl” education. GGAST provides a rigorous college prep academic program, combined with leadership training and extra-curricular activities that fill girls with confidence that they can pursue their dreams of university education and fulfilling and impactful vocations. After schools around Rwanda were closed in March due to COVID-19, the academy began providing its curriculum online, working with students in different parts of the country to resolve challenges with their internet access. GGAST is exploring ways to support the wider community, having received multiple requests from other students to join its distance learning program. One way has been to provide lessons online through a newly launched YouTube channel. In addition the 42-acre teaching farm that provided food to students and teachers at GGAST is now providing food to the most vulnerable people in the wider community.
Sahar
As with many organizations, Sahar’s work has been complicated by the ongoing COVID-19 pandemic. In March, Afghanistan’s Ministry of Education closed schools and because many of Sahar’s programs operate within Afghan public schools, this meant suspending in-person programming. Through a partner, Sahar has continued its programs remotely via WhatsApp. Sahar’s Men as Partners in Change Program and Early Marriage Prevention Program now deliver training and COVID-19 response information online. In addition to adopting a remote model of programming, Sahar has also distributed care packages with COVID-19 necessities like hand sanitizer and face masks. Looking forward Sahar sees addressing gender equality as fundamental to recovering from the pandemic. In Afghanistan, many girls likely will not return to school in the fall. There are growing concerns that many girls will face early marriage due to their families’ financial struggles. Furthermore gender-based violence globally has increased, as women have been forced into lockdown with their abusers. Sahar sees gender as a challenge of COVID-19 response, as well as an opportunity. Girls are an invaluable resource to their families, communities, and countries. By promoting the right of girls to receive an education (even and especially within a pandemic), Sahar is promoting the development of a peaceful and resilient Afghanistan.
Back to Top
Organization Profile
More than 20 Years After Founding a School for Former Child Soldiers in Rural Uganda, Pilgrim Africa Continues to Respond to Children’s Needs During Global Pandemic
By Joanne Lu

(Pre-COVID-19) Students work on their lessons outside Beacon of Hope, a secondary school in Soroti, Uganda. The school was originally founded by Pilgrim Africa for former child soldiers.
Photo: Pilgrim Africa.
Calvin Echodu was a reporter in Uganda in the mid-1990s when he decided he had to do more to help. Joseph Kony’s Lord’s Resistance Army (LRA) rebel group was sweeping through northern Uganda, brutalizing civilians, abducting children to become child soldiers and sex slaves and forcing families to flee their homes and become refugees in their own country.
Echodu and some friends solicited help from churches so that he could bring relief supplies to displaced families in camps every time he went to report in the north. Thus, Pilgrim Africa was unofficially born in 1998. In 2001 it was officially registered as a non-governmental organization, continuing to carry out relief work in northern Uganda, especially providing trauma support for abducted children and former child soldiers.
From its very inception, Pilgrim Africa has responded to the needs on the ground. As those needs have changed, so has Pilgrim Africa, constantly evolving to meet the needs expressed by community members. For example, as the war in northern Uganda settled down, Pilgrim Africa transitioned from relief work to helping more than 1,000 families resettle back into their villages that many of them hadn’t seen in a decade because of the war. And in 2005, they founded a secondary school in Soroti, called Beacon of Hope, for children recovering from the war.
Initially, Beacon of Hope was founded as a remedial boarding school for former child soldiers, abductees or victims of rape camps. According to Echodu, who directly oversees the school’s operations, a considerable number of children, who were directly victimized by the war, were too far behind in their schooling to jump back into regular secondary schools. But they were also too old for primary school. So, with the support of donors, Beacon of Hope offered these students free, quality education, with an agreement that the students would complete extra coursework to catch up with their peers.
Echodu says that in the first four to five years, Beacon of Hope served about 2,000 students. In addition to providing a quality education and a safe place to live and grow, they made sure to provide trauma support to both their students and the community, with social workers, counselors, and a medical facility inside the school.

(Pre-COVID-19) Students at Pilgrim Africa’s Beacon of Hope school in rural Uganda share a laugh outside of classes. Photo: Pilgrim Africa.
In 2014, the last child soldiers graduated, but by then Beacon of Hope had opened its doors to other students, continuing to offer free boarding education to students who otherwise would not have access to schooling of that quality. In particular, girls always make up about half of the student body. The school provides career guidance and counselors specifically for girls, to address their needs through a gender lens, empower them, guide them and ensure they are in a safe environment to reach their full potential.
Beacon of Hope was also one of the first schools outside of the country’s capital, Kampala, to focus on STEAM education: science, technology, engineering, arts, and math. Echodu says that because Uganda is a young country in terms of industry and development, STEAM education sets up both their students and the country for future success. “We train kids in that direction so they will be innovators and provide the solutions, jobs and development that the country needs,” says Echodu.
Echodu says they’ve already seen some of that success in action. As of the end of last year, Beacon of Hope has educated more than 5,400 students since its founding, many of whom have gone on to serve their community and country. Some have become teachers and engineers, and several have gone on to become medical doctors, including a few who work at the local hospital. Last year, the school’s robotics team won two gold medals at an international competition.
But running a school like Beacon of Hope hasn’t been without its significant challenges, says Echodu. First, there has always been the academic challenge, as many of the students come from poor academic backgrounds – and traumatic ones, too. It’s up to Beacon of Hope’s talented teaching staff (all of whom are Ugandan) to make each of their students academically competitive.
Second, he says, running a STEAM school in a rural part of the country has presented its fair share of obstacles, as well. For example, especially in their early days, they ran into problems with getting consistent and affordable access to electricity, adequate internet connectivity, logistics and infrastructure.
Third, there’s always the challenge of funding. Up until two years ago, says Echodu, Beacon of Hope was able to raise enough support to provide full scholarships to all of its students. What that meant, in exchange, was that they had to accept fewer students because of funding constraints. These days they accept paying students; the high quality education they offer is in great demand. Moving forward, they want to accept more students, increase their staff and adopt a more sustainable funding model, including encouraging successful alumni to participate in fundraising.

(Pre-COVID-19) Students walking to their classes at Beacon of Hope school in rural Uganda. Photo: Pilgrim Africa.
This year, the COVID-19 pandemic has brought its own set of challenges. Echodu says that Beacon of Hope is one of the few institutions that has been able to continue paying its teachers their full salaries – although, how long they’ll be able to keep that up depends on fundraising. With the help of a $23,000 grant from The Allen Family Foundation, they’ve also been able to purchase tablets and internet access for all 80 of their A-level candidate students (those preparing for university) so they can participate in online classes. The Church of the Redeemer in Chestnut Hill, Boston, has also been a visionary supporter during the pandemic, providing a $28,000 grant for COVID-19 relief, faculty expansion, and other improvements to the Beacon of Hope library and IT lab. Meanwhile, teachers are checking up on the other students, especially girls, and making sure that they have access to books and other educational materials. “It has been a challenging period,” says Echodu.
Thankfully, not everything has been put on hold by the pandemic. The school is still on track to purchase the property it had been leasing, and Pilgrim Africa has been able to continue some of its malaria programming, which it began in 2008. In addition, the organization has created a website and provided personal protective equipment to the national task force responding to the pandemic, as well as food and aid to families in lockdown. As it was from the beginning, Pilgrim Africa is responding to the needs on the ground.
Back to Top
Goalmaker
For Judithe Registre of Girl Rising, Stories Shape the Future
By Amber Cortes

Photo courtesy of Girl Rising.
I have this funny way of introducing myself,” says Judithe Registre, Vice President of Programs at Girl Rising. “I describe myself as Haitian-born, American-made, and globally-centered.”
As a child growing up in Haiti, she dreamed big.
“I was one of those people who kind of always knew, walking from school along the dusty Streets of Haiti, that I would travel the world!”
For Registre, that global journey started when she immigrated to the US at the age of 12, continued when she completed her post-graduate work in South Africa and began a career in international development. It has since brought her all over Africa and to over a dozen countries including Egypt, El Salvador, India, Indonesia, Nepal, and Vietnam.
It’s also no surprise to Registre that she now works for Girl Rising, an organization that’s harnessing the power of storytelling to change the way the world values girls and their education —because she’s been fighting for girls’ rights since she was eight years old.
“I joke about the idea that I’ve always been a feminist long before I understood what the word feminism was,” she explains.
It all started one day in school when Registre and the other girls in her class were taught to learn how to wash—“with one exception, the boys didn’t have to do that. And I remember being very confused about being asked to go learn how to wash my clothes when the boys didn’t have to.”
“And I became, I don’t want to say adamant as much as I needed answers. And it wasn’t enough to say well, that’s just the way it is.”
The moment turned out to be a defining one for Registre’s life and work.
“It started to actually help me to really look at the world and the role that people were playing in it—how did they come to play this role? Did they accept it? Did they sign up for it? And then feeling like we have the freedom or the choice to play a different role.”
In her higher academic work, Registre chose to study philosophy—a decision that surprised many around her. But for Registre, philosophy was a lens to understand the world more broadly—a tool combining economics, political science and anthropology that served as a framework to begin asking questions about the world.
As Registre began asking questions from a feminist perspective, she became more acutely aware of how educating girls at a young age empowers them to rise above their circumstances and shape their own future.
“Because those vulnerabilities start when they are a girl. And if you wait to invest in women and not in girls, you’ll be fighting a battle for generations to come around this issue of gender inequity.”
To that end, Girl Rising seeks to plant the seeds that can put a girl on a “lifelong path” to continued learning—even if their circumstances become limited by say, an arranged early marriage. But for Girl Rising, it’s not enough for girls just to be educated. At the end of the day, says Registre, it’s about affirming their basic humanity, like the struggle currently playing out globally as U.S. protests from the Black Lives Matter Movement gain international attention and momentum.
“If you look at women, or the Black experience, the experience of Indigenous people—just the experience of being excluded in any society, it is a historical struggle for existence, the right to live and the right to be considered as a person.”
Registre recognizes that in a world where racism and the forces of inequity are everywhere, this struggle takes time, resources, and attention. “So, how do we build a world that values girls at the core of the humanity when the entire infrastructure, the ecosystem, the wallpaper, the oxygen in the air, reinforces the idea that you are not human? This is the challenge.”
The COVID crisis has, of course, exacerbated this challenge, bringing disruptions at a global, community, and household level. The rug has been pulled from under our feet, and particularly vulnerable communities—those with “social pre-existing conditions,” as Registre puts it, include women and girls.
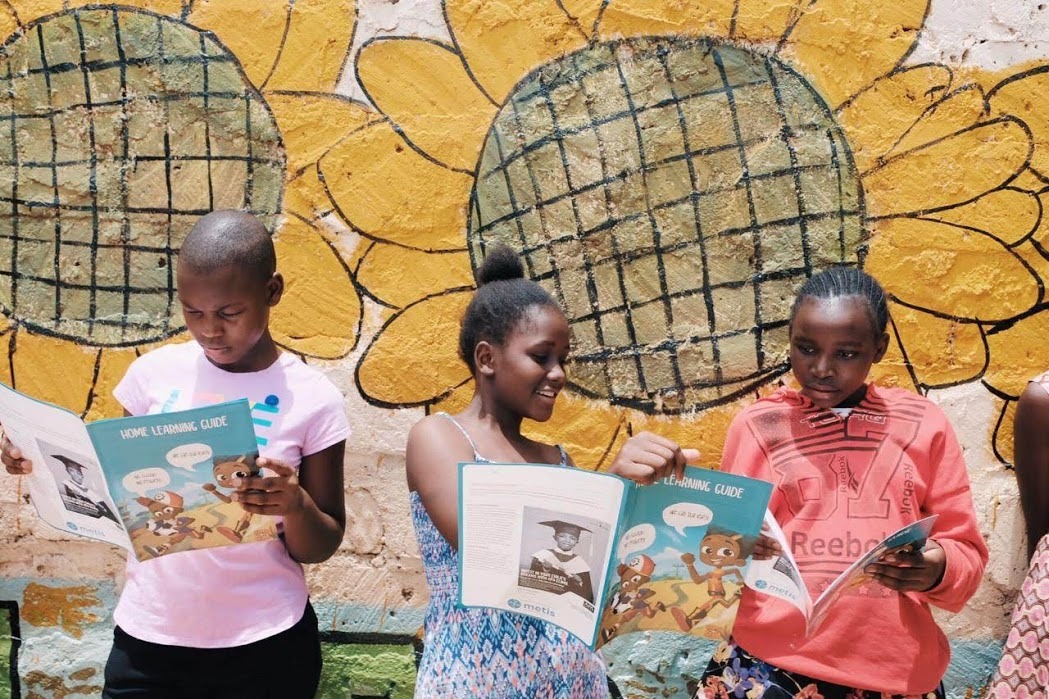
Even with schools closed around the world, learning continues. Girl Rising partner Metis Collective developed a Home Learning Guide, which is being put to good use in Kenya. Photo by Metis Collective, and provided by Girl Rising.
Progress being made towards the UN’s Sustainable Development Goals (SDGs) for education like in Kenya, where girls were increasing in school completion and enrollment rates, threatens to be rolled back with the closure of schools. Not long ago, female genital mutilation (FGM) and early marriage were on the decline. But now, domestic violence and child abuse are increasing.
In addition, Registre adds, the burden of the care economy is still very gendered, and responsibilities like tending the house or caring for the sick falls on women and girls, who occupied these roles before the pandemic.
But Girl Rising is thinking two steps ahead and keeping girls close to education even during a pandemic by supporting community-created solutions in the 11 countries where they deliver on-the-ground programming. For example, they’re working with local mentors and teachers in Guatemala to redesign their programs to offer affordable and accessible educational radio programming in Guatemala.
They’re also returning to the core of what they do—elevating the humanity of girls by empowering them to tell their own stories—in their own voices. In June Girl Rising launched the My Story Storytelling Challenge. The challenge is open to all, and the goal is to amplify the voices and experience of people in communities who are impacted by COVID-19, and inspired to help. It is important, says Registre, to be documenting this current historical moment as it happens, and not just as an afterthought.
The project already features several stories, from a dance school in Nigeria, to high school students in South Africa organizing to protest gender-based violence. Registre says the point is to highlight the hopes and aspirations of young people—since they’re the ones who will be shaping the discourse and solutions to the impacts of the pandemic for years to come.
“The ideas of hope and optimism used to be elusive things. But in this curious moment, this strange new climate, we need dreamers, we need optimists. We need those who are hopeful because they will put the creative energy in to stay the course.”
Registre is a firm believer in the power of stories: “When we talk about the software for the human operating system,” she says, “I think that software is story.” The stories we tell ourselves form who we are—and give power to those who get to tell them—like in religion, nation-building, and even the story of America, which is changing and unfolding even now into a much more complex story than many people learned in history class.
All her life, Registre’s always heard stories that conflicted with the reality she knew and understood to be her own—like Haiti’s reputation as the poorest country in the Western hemisphere, ravaged by earthquakes and AIDS, or Congo being dubbed the ‘Rape Capitol of the World.’ That’s why she thinks it’s crucial for people to shape their own stories of who they are and what their lived experience is.
“When we talk about racism and gender inequity, I started to realize how things are shaped for us, how it becomes this frame that we package an entire population of people in, not really displaying the humanity of who those people are.”
Story equity is the practice of stepping back, of listening, and of questioning your role as a storyteller who is “a voice for the voiceless,” and instead shifting that power dynamic to being a story facilitator—to finding ways to empower and support those who need to tell their own stories.
“And I always used to sort of ask that question when I was in the ground working in Congo: If I were this person, would this story show and display me in all my dignity? Would this be a story that I tell about myself?”
Narrative justice is the result of true story equity—”the creation of a cultural awakening that seeks to shift representation, voice, and agency,” as Registre writes here.
When it comes to the international development sector, it’s so easy to fall into the role of a well-meaning advocate, wanting to tell the story of a marginalized person or community.
“I think we tend to be default operators of systems because we never stopped to reflect and say, ‘What was this designed to do? Does it still serve its purpose?”
“We need to be thinkers and designers of new systems,” Registre insists. “We need to rethink international development to really ask ourselves, what is our role in the world? And what should we do to serve in that respect in our work. And what does that look like? Our engagement in the true meaning of partnership is that power is understood to be shared after all, right? “
Despite the threat of COVID-19 impacts, Registre keeps optimistic—in fact, she thinks the current challenge will force us to change in ways that are more sustainable in the long run, and this long-overdue shift is happening much faster than expected due to the pandemic.
“There’s this kind of acceleration to change that is fast-tracking us to reconsider and redefine and reimagine. We’re entering a completely different stage in our historical development as a human society globally, and the COVID-19 reality is helping us to see this.”
Back to Top
Welcome New Members
Please welcome our newest Global Washington members. Take a moment to familiarize yourself with their work and consider opportunities for support and collaboration!
Friends of WPC Nepal
Friends of WPC Nepal is a fundraising organization that seeks to prevent human trafficking as well as protect and empower at-risk women and children in Nepal through awareness programs, education scholarships, job training and the Safe Home. Our strategy is focused on prevention, protection, and empowerment. We work in partnership with our sister organization, Women’s Protection Center Nepal, which is strategically based in Hetauda near India where many victims are forced to work in brothels, households and circuses. friendsofwpcnepal.org
Back to Top
Member Events
August 13: Construction for Change Virtual Benefit
August 18: World Affairs Council: Europe in the Age of COVID-19: Public Health, Social Solidarity, and the Role of Government in a New International Environment – Virtual Program
August 21: Global Visionaries: Guatemalan Cook-along
August/September: Global Leadership Forum is still accepting applications for Fall 2020. Contact Kim Rakow Bernier for more information, rakow.bernier@gmail.com or (206) 250-6383,
September 2-3: Priority deadline to register for the Social Innovation Accelerator Program (AST 2020) through the UW Evans School of Public Policy & Governance
September 12: Friends of WPC Nepal: Hope For Freedom Gala 2020
Back to Top
Career Center
Marketing and Communications Manager // Splash
Program Lead – Capacity Development and Inclusion // Forest Stewardship Council (FSC)
Impact & Learning Associate // Days for Girls
Check out the GlobalWA Job Board for the latest openings.
Back to Top
GlobalWA Events
August 21: Education and COVID-19 in the Global South
September 16: Final Mile Event: Kicking off a US chapter of the International Association of Professional Health Logisticians (IAPHL) and the COVID-19 work of Restart Partners
Back to Top
PRESS RELEASE: Americares Responds to Explosion in Beirut
Posted on August 11, 2020.
Stamford, Conn. – Aug. 11, 2020 – Americares is sending nearly 60 tons of medicine and supplies to hospitals and medical facilities in Lebanon where an explosion in Beirut’s port last week left 150 people dead and injured at least 5,000 others.
Americares is sending a series of shipments, valued at nearly $900,000 to partner organization Anera, which supports over 450 health facilities and social service organizations throughout the country. Most of the medicines and supplies, including IV fluids and anesthesia medicine, are destined for hospitals and clinics treating survivors of the massive explosion. The blast comes on the heels of a political and economic crisis, a mounting refugee crisis, increasing poverty and a worsening COVID-19 outbreak in the country.
Continue Reading
July 2020 Newsletter
Welcome to the July 2020 issue of the Global Washington newsletter.
IN THIS ISSUE
Letter from our Executive Director

Recently, a colleague asked what I am optimistic about during these troubled times, and I couldn’t find an answer. The immediate and long-term impacts of COVID-19 are devastating and have widespread global implications. In addition to an unparalleled health crisis, the resulting economic downturn and loss of livelihoods has been severe.
As a result of the pandemic, an estimated 71 million people around the world will fall into extreme poverty, defined as living below $1.90 a day, undoing years of progress on this front. Those most vulnerable are low-income families in developing countries. In certain regions, the loss of income and inability to buy food represents a far greater threat than exposure to the virus.
Despite feeling the weight of this moment and the enormity of the challenges ahead, I am honored to lead a network of 160 incredible organizations that are responding head on to the challenges COVID-19 poses to people in the Global South. Our members are working every day to strengthen the safety net for families in need and bolstering recovery efforts. Seeing the speed and breadth of their collective responses, I can honestly say that I have hope for the future. I encourage you to read more about our members’ work, and let me know what makes you feel inspired and hopeful.
Over the past few months, we reported on the global health implications of COVID-19, as well as the impact on refugees, food security challenges, and the importance of sustainable clean water access. In this issue, you will learn more about the economic implications of this pandemic and how our members are supporting markets and communities through these overlapping challenges.
When we seek to understand solutions rather than focus only on the enormity of the problems, we can regain our optimism. Global Washington will continue to amplify the solutions our members are implementing and showcase what is working around the globe as we fight this pandemic together.
Kristen Dailey
Executive Director
Back to Top
Issue Brief
Navigating the Economic Fallout of Covid-19 and Building Back Better
By Joanne Lu

Women from a community in Quezon City, Philippines line up to enter a market as the local government strictly imposes social distancing in public places. They also received flyers from IDEALS and Oxfam containing relevant information about COVID-19 and essential tips on how to cope with the enhanced community quarantine. Credit: Ideals
The COVID-19 pandemic is an unprecedented global health crisis. But now it appears that by some measures it will be an even greater and more lasting economic crisis, particularly for the poor in developing countries.
Since 1990, nearly 50 million people have climbed out of poverty every year. It’s one of the greatest achievements of the millennium. But now, the pandemic has plunged the global economy into the deepest recession since World War II, according to a recent report by the World Bank. And an estimated 71 million will likely be pushed back into poverty for the first time since 1998, a new UN report warns. According to the World Bank, this is the first global recession to be triggered solely by a pandemic.
So far, economic projections have shown worse outcomes for advanced economies than developing countries, because the pandemic surged in wealthier regions first, causing lockdowns that suspended and shuttered businesses. But from the beginning, economists have warned that there remains a great deal of uncertainty around the pandemic and its impacts. And, lower-income countries are likely to suffer severe and more lasting impacts because many already have less health-care infrastructure, weak social safety nets, large informal economies, a higher dependence on trade and more people living at or around the extreme poverty line. Now that the pandemic is beginning to surge in countries across South America, South Asia and even Africa, economists and development experts are intensifying their calls for global support and innovative interventions. With lockdown measures in place and business activity disrupted, people who were dependent on meager daily wages are facing hunger and exploitation. And as 90 percent of students worldwide have been kept out of classrooms by school closures, developing countries’ future growth potential is also being severely undermined.
Even before the pandemic, many emerging and developing countries struggled to provide adequate social protections for their citizens due to a lack of resources rooted in problems such as over-indebtedness and poor governance. Now, perhaps more than ever, social safety nets are crucial for keeping households afloat, which is why many humanitarian and development organizations, like Oxfam America and Mercy Corps, have scaled up their food assistance, cash transfers and voucher programs.
Oxfam is also advocating for an “Emergency Rescue Package for All” that would cancel trillions of dollars in debt for developing countries and would increase the funds available to them by at least a trillion. With more funding, countries could expand their social protection programs, including unemployment insurance. But developing countries are facing a serious hurdle with important interventions like unemployment insurance: a huge number of people work in the informal economy, or “off-the-books.” According to the UN’s International Labor Organization (ILO), more than 2 billion people globally make their living in the informal economy; 93 percent of them are in emerging and developing countries. In Africa, nearly 86 percent of employment is informal. This means that governments are having trouble targeting their economic aid when a large portion of small businesses and workers do not file taxes or even have access to formal banking. In a recent report, Mercy Corps wrote that “informality continues to be a significant factor determining individuals’ ability to adapt.” The UN’s Sustainable Development Goals 2020 report estimates that just in the first month of the pandemic, workers in the informal economy saw their incomes drop 60 percent.
Given the need to rapidly deploy economic assistance across the board – including to informal workers, many of whom are the poorest of the poor – some governments and organizations have turned to digital payments, mobile money, and community-based virtual currency to help families receive aid and purchase essential items, like food and soap, without using cash while social distancing. The Mifos X open source banking platform by Mifos Initiative, for example, allows governments to quickly and affordably open cloud-based bank accounts. Individuals, many of whom were “underbanked,” can then receive cash and benefit payments through these accounts, and businesses can access credit and reschedule loans. In addition, Google and the Bill & Melinda Gates Foundation recently also announced Mojaloop, a free, open-source payment platform that connects many different banking and payment systems across a country. Although the need for financial inclusion is time-sensitive during the current crisis, these digital solutions will help developing countries continue to grow over the long run.
An unprecedented characteristic of the COVID-19 economic crisis is how widespread the impact has been. Because advanced economies have also been battered by the pandemic, they’re less able to help sustain emerging and developing economies through trade. Migrant workers in wealthier countries are also experiencing a loss in wages, meaning they’re unable to send as much money home to their families. For developing countries, these remittances are an essential source of income. The World Bank is predicting a 20 percent drop in remittances this year, the sharpest decline in recent history. In Africa, a hit to tourism is also “decimating” the livelihoods of middle-class workers, who were driving the continent’s economic growth, according to a recent article in the New York Times.
As Microsoft President, Brad Smith, recently wrote in a blog post, “the pandemic has shined a harsh light on what was already a widening skills gap around the world – a gap that will need to be closed with even greater urgency to accelerate economic recovery.” Microsoft’s answer to this problem is a new “global skills initiative” that will help 25 million people around the world gain digital skills by the end of the year. The initiative will identify in-demand jobs and the skills needed to fill them, provide free educational content to develop those skills, and provide low-cost certifications and free job-seeking tools. But digital skills aren’t the only path forward. Einstein Rising, a business accelerator for social entrepreneurs in Africa, has launched online “Skills for Change” workshops that teach practical, income-generating skills, such as how to make liquid soap and petroleum jelly for dry skin.
But perhaps more than anything, the pandemic is highlighting just how important it is to develop strong partnerships in our interconnected world. The most vulnerable among us will not be able to survive the impacts of the pandemic without global support; at the same time, the pandemic has made it clear that no one is truly safe and secure unless all of us are. Organizations like Global Partnerships, Upaya Social Ventures and 3rd Creek Foundation are leaning into their partnerships with social enterprises and other organizations in order to help keep everyone – investors, organizations, businesses and households – afloat in these trying times.
Without a doubt, the COVID-19 pandemic is an economic shock of historic proportions that will reverse much of the progress the world has made toward eradicating poverty. However, with innovative solutions and global cooperation, this crisis also presents the world with an opportunity to build back better if we extend the interventions being implemented now into a post-pandemic society. With stronger social safety nets for everyone, financial inclusion through technology and new skills for a changing global economy, perhaps a more equitable society awaits.
The following GlobalWA members are working to address the economic impacts of the COVID-19 pandemic in developing countries.
Awamaki
Awamaki is a small non-profit that connects Andean artisan weavers with global markets to create economic opportunities and improve social well-being in rural Peru. Peru has had the longest lockdown in the world, with borders closed and tourism, transportation, and commerce shuttered for over three months. Awamaki’s partner artisans and their families rely almost entirely on tourism for their incomes and as a result, their villages have been severely affected by the lockdown. Awamaki is fundraising for emergency food relief so the artisans can feed their families while there is no work. The organization is also supporting 160 artisan women and their families with food donations. Additionally, Awamaki is looking for creative new opportunities, including supporting the artisans in making face masks to prevent transmission of the virus that causes COVID-19. Additionally, they have been hosting weaving demonstrations on Zoom, a new way to bring income to their families.
3rd Creek Foundation
Through grants and impact investing, 3rd Creek Foundation supports early stage programs that create sustained economic improvement and dignity for the ultra-poor. The foundation’s recent fundraising campaign, #raise20run20, will support its partner organizations including non-profit organizations that run entrepreneurial training programs as well as small businesses that employ the ultra-poor with dignified jobs.
Bill & Melinda Gates Foundation
The Bill & Melinda Gates Foundation has made critical investments in speeding up development of new tools to address the COVID-19 pandemic, including advanced diagnostics, therapeutics, and vaccines. In addition, the foundation has highlighted the disproportionate impact the pandemic is having on women’s health and economic well-being. Recommended policy actions include ensuring women are essential recipients of financial aid and emergency cash transfers, directing stimulus dollars toward women-owned businesses, increasing women’s access to cell phones in order to manage their money digitally, encouraging flexible work arrangements, and including diverse experts and leaders in decision-making.
Capria
Capria is a global impact investment firm managing multiple funds that accelerate the flow of capital to deliver superior returns in emerging markets. Capria holds COVID-19 workshops with its fund managers twice a week to share knowledge and learn from the experience of its partners across the network. The company has found investments in essential products and services to bottom-of-the-pyramid consumers to be a resilient strategy because they serve critical needs even during times of uncertainty.
Dalberg
Dalberg has been actively supporting its clients globally on how to respond to the COVID-19 pandemic. This has involved helping large foundations pivot their strategies and grant-making; assessing vaccine discovery efforts for improved access in the developing world; designing bridge finance facilities; and, increasingly, adapting to the “new normal.” A survey Dalberg conducted on leaders at various global philanthropic organizations provides insight into their shifting priorities around the current pandemic. Another report Dalberg co-authored with World Wildlife Fund details the root causes of the COVID-19 crisis and recommends ways to mitigate future pandemics.
Global Partnerships
Global Partnerships is an impact-first investor dedicated to expanding opportunity for people living in poverty. The organization makes loans and early stage investments in social enterprises that deliver market-based products and services that empower people to earn a living and improve their lives. GP supports its partners in meeting the needs of the most vulnerable during the pandemic. For example, BRAC International, a global microfinance network in Liberia, Tanzania, and Uganda has begun conducting telephone outreach to clients, disseminating health guidance through radio broadcasts, deploying a rapid income and food security assessment to better understand client needs, and proactively linking its clients to non-profit and government resources. Another, Acceso El Salvador, is an agricultural enterprise that purchases goods from smallholder farmers and fishers. Acceso has immediately adapted its technical assistance to focus on pandemic-safe practices while providing farmers with frequent updates on which produce is in high demand. A third partner, Friendship Bridge in Guatemala, responded to the drop in revenue for their female artisan clients by working with them to produce and sell face masks to meet the growing global need.
Foster School of Business (University of Washington)
For over a decade, the Foster School of Business has worked with the Self-Employed Women’s Association (SEWA), “a trade union that promotes the rights of self-employed female workers and aims to organize them for full employment and self-reliance,” according to a former UW Global Business Center Global Consulting Project participant. The partnership brings MBAs together with small business owners in rural India, where students complete projects for the organization as part of their course. SEWA members have produced over half a million face masks (as of April) in response to the coronavirus pandemic.
Landesa
As a global leader in land rights, Landesa is positioned to assist its partners in government and civil society in responding to COVID-19. The organization is leveraging its networks in Asia and Africa to provide resources and expertise for local partners on the front lines of this global health crisis. In Liberia, Landesa is using its nationally broadcast radio program to educate the public on health, hygiene and social-distancing measures to prevent transmission of the virus. In Tanzania, Landesa is adapting a mobile application, “Law On Your Palm,” which connects rural women with access to legal services, to be used to share information about COVID-19. And in Myanmar, Landesa is helping to equip the Forest Department with protective masks and gloves for use by department staff carrying out essential fieldwork.
Mercy Corps
Mercy Corps works in more than 40 countries in the Americas, Africa, Middle East and Asia, providing assistance to communities facing crises of all types, including vulnerable people whose circumstances are being made worse by the pandemic. Mercy Corps is responding to the urgent needs, while also investing in long-term solutions that build resilience to future crises. To support the most vulnerable families, Mercy Corps is providing emergency cash assistance so they can cover essential expenses such as food, water and rent. Cash also jumpstarts the local markets and businesses, enabling them and the larger economy to recover. Additionally, Mercy Corps helps small businesses adapt and recover after a crisis, as they are often both the engines of the economy and the most vulnerable to economic disruptions. Through technical support, grants and mentorship, the agency helps businesses get back on their feet, increase their chance of long-term success, and become better prepared for future disasters. A key aspect of Mercy Corps’ work is helping individuals and business owners access financial services and increase financial literacy, so that they have the tools and skills to save for the future, borrow to invest in their businesses, and manage risks no matter the crisis.
Moving Worlds
In partnership with SAP, leading impact investors, and social enterprise thought-leaders, the MovingWorlds Sustainable Growth of Revenue for International Development (S-GRID) program helps social enterprises, and the individuals within them, to create sustainable revenue streams by partnering with the corporate sector and connecting into global value chains. As we begin to rebuild our post-COVID world, there is an unprecedented opportunity to go beyond the status quo to build more just, equitable, and sustainable global systems.
Oxfam America
Oxfam America estimates that half a billion people could be pushed back into poverty by the COVID-19 pandemic. During a time of extreme global inequality, this could set back the fight against poverty by a decade, and as much as 30 years in some regions such as sub-Saharan Africa, The Middle East and North Africa. To address the immediate need for economic support, Oxfam is providing cash and in-kind food assistance to those who need it in more than 15 countries around the world, including for refugees, displaced people, and vulnerable families, including in South Sudan and Central African Republic. In the Dominican Republic, for example, Oxfam is working to transfer cash to 4,000 families (benefiting some 20,000 people) to buy basic goods. Oxfam is also partnering with small-scale food producers to amplify their voices in the call for global action on the looming food crises. Oxfam understands that addressing COVID-19’s economic impacts requires a multi-sectoral response and the cooperation of local and international organizations, corporations and governments. At the global level, Oxfam has called for the international community to fully fund the UN’s humanitarian appeal and cancel debts so that poor countries are able to focus on critical needs. Oxfam has also called for an emergency rescue package for all that provides cash grants to those who have lost income and creates at least a trillion dollars in international reserves to dramatically increase resources available to countries.
Pangea
Pangea has supported its community partners around the world by offering additional flexibility in their grant timelines and supporting organizations as they have shifted their programs toward COVID-19 response. Child Empowerment Program in Uganda, for example, has been producing thousands of masks, sewn by graduates of its tailoring program who received training at CEP’s vocational school (with previous funding from Pangea). They will distribute the masks free of charge to health workers and women who are still struggling to sell vegetables in the market to support their families.
Rise Beyond the Reef
Rise Beyond the Reef bridges the divide between rural remote indigenous Fijian communities and the outside world, promoting women as leaders of their communities on the frontlines of climate justice. The organization has been working with its partners in Fiji to distribute protective COVID-19 kits with washable masks, gloves and disease awareness infographic flyers. Additionally, Rise Beyond the Reef has helped distribute basic food rations to remote partner communities and marginalized areas inside Fiji’s restricted areas to prevent them from traveling to town centers for shopping. And finally, the organization has distributed raised seedlings to partner communities to help boost food security.
Spreeha Foundation
Spreeha strives to break the cycle of poverty for underprivileged people by providing healthcare, education, and skills training. COVID-19 has forced the foundation to temporarily close education and training services in order to ramp up its healthcare response, including telehealth. Spreeha is also working closely with the government of Bangladesh in providing health awareness messaging and door-to-door coronavirus screening services.
Upaya
Upaya Social Ventures fights extreme poverty with dignified jobs and believes job preservation and job creation are crucial to the COVID-19 recovery. To date, Upaya has invested in 21 early-stage businesses that provide jobs for over 17,000 people in the poorest regions of India. To understand how the pandemic is impacting those vulnerable communities, Upaya surveyed a sample of job holders by phone and found that the majority of those surveyed were able to earn money during the lockdown, thanks to their connection with Upaya portfolio companies. To combat the devastating effects of the pandemic, Upaya launched a three-wave strategy in April, starting with helping their existing portfolio companies survive the economic downturn by facilitating access to relief programs and virtual peer learning sessions. The team has since begun deploying revenue-based financing to the companies in its portfolio to provide the liquidity needed to maintain operations and preserve jobs. Upaya has also promoted the direct-support campaigns run by its portfolio companies to assist people who lost their ability to earn during lockdown. Looking toward the recovery, Upaya is building a pipeline of promising new companies and has adapted its annual Accelerator Program into a series of virtual workshops. Upaya has also implemented a streamlined investment process to rapidly extend investments to fill the small business financing gap that has been worsened by the pandemic. The team intends to invest in at least six new companies this year that are creating dignified jobs to fuel the COVID-19 recovery.
Back to Top
Organization Profile
Collaboration Enables Impact Investing Firm Capria to Support Thriving Entrepreneurial Ecosystems, Even Amid a Global Pandemic
By Penny Carothers

Susana Garcia-Robles speaking alongside Mexican fund managers on impact investment strategies.
Photo courtesy of Capria.
Early in her career Capria’s Susana Garcia-Robles was on the forefront of developing the private equity and venture capital markets in Latin America and the Caribbean while working with the Inter-American Development Bank. She recalls skeptical governments asking—so often she lost count—“[Is] innovation, entrepreneurship, and venture capital relevant to a region mired in poverty? Aren’t they just entertainment for rich young people?”
It wasn’t just governments that were confused by the role of impact capital in development. When the term “impact investing” was coined in 2007 to describe the goal of turning a profit while creating positive and measurable social and environmental impact, early investors lacked consensus on both methods and expectations. Some clarity came in 2009 when Jessica Freireich and Katherine Fulton of the Monitor Institute described the difference between “financial-first investors” and “impact-first investors.” (Long story short: it appeared that achieving both at the same time was not quite possible).
Today, investors of all stripes participate in an ecosystem that has grown significantly even at this early stage of its development. The 2020 Annual Investor Impact Survey put out by the Global Impact Investing Network (GIIN) estimated the size of the market to be $715 billion in assets worldwide, invested by more than 1,700 organizations. Impact investors now challenge the perceived incompatibility between social and financial gain, though consensus is by no means universal.
“If you don’t get returns, economies don’t grow.”

Capria partnered with its anchor investor, International Finance Corp., to be among the first to embrace IFC’s Operating Principles for Impact Management. Photo courtesy of Capria.
Founded in 2015, Capria has always rejected the assertion that investors must choose between social or environmental goals and financial returns. Capria’s successes in this area are a strong argument that it is possible to meet the dual goals of impact investing without compromising on either side. With a global network of funds representing $400 million in assets under management, Capria invests in early-stage venture capital, private equity, and other debt and equity funds in 37 countries in Latin America, Africa, and Asia through local fund managers and in some cases through direct investments. Their methods are built on lessons learned by investing in both developed and emerging economies. Capria’s leadership has deep experience in US-based technology companies, as well as through an early stage venture capital fund, Unitus Ventures.
“In a nutshell, we’re not an impact-first investor,” says Garcia-Robles, Capria’s Venture Partner. “Financial and social/environmental returns are at the same level of importance. How do we do that? Our ‘secret sauce’ is our collaboration.”
Capria leads the largest network of fund managers in what they term a pragmatic and collaborative approach that draws deeply on best practices in venture capital, impact measurement, and environmental and social governance (ESG) management. Capria’s cohort of fund managers span 22 countries and have a range of industry experience. When fund managers join the Capria Network they access professional peers as well as proprietary tools available through Capria Quantum, a system that includes templates, agreements, assessment tools, and resources of all kinds to increase fund managers’ knowledge and effectiveness.

Capria’s 7th investment cycle culminated at the Seattle Impact Hall and included managers from Brazil, 3 countries in Africa, Singapore, and India. Photo courtesy of Capria.
Capria uses this model of a capacity-building network because it believes that the most successful early-growth investing must be led by local fund managers and teams that know their own markets and opportunities. As Garcia-Robles says, “[This model] is very effective because you’re empowering local teams who in turn empower local entrepreneurs.” Fund managers often take board seats on the companies they invest in, and any knowledge Capria shares with their fund managers can then be used to strengthen their portfolio of companies.
Using this model, Capria envisions “thriving entrepreneurial ecosystems” in dozens of new markets in order to realize its long-term goal of deploying $1 billion in capital to impact 100 million lives.
Crisis management and COVID-19
Capria’s approach has served the firm well during the current pandemic. Susana Garcia-Robles, who serves as Capria’s crisis manager, said, “When Covid hit, we had to move fast…. [Capria’s] vision comes through having been through many crises. We know that behind any crisis there also are new opportunities if you are realistic and pragmatic about going after them.”
After an intensive two-week period of information gathering and assessment at the very start of the pandemic, Capria began to create more tools to add to Quantum. These included a crisis preparedness tool, which was vetted and shared widely outside the Capria network, as well as a financial matrix that fund managers could use to analyze a business’s position and runway for exiting the crisis.
Capria has doubled down on the principles key to its model since the beginning. Twice a month Capria holds COVID-19 workshop meetings with its fund managers. Topics have ranged from lessons learned from past crises, to how to pitch investors during a pandemic, to legal aspects of the pandemic. All build on the shared knowledge and experience of the partners across the network.
Unexpected losers and not-so-obvious winners
In the beginning, the knee-jerk reaction to the crisis was the belief that every digital business would pull out of the crisis and every traditional business would not. When Capria’s network looked more closely at their portfolios and deal pipelines they saw that this was inaccurate. To highlight crisis management best practices, Capria held a workshop to showcase “unexpected losers and not-so-obvious winners,” including an app-based ride service in India that lost 70% of its revenue in the early weeks of lockdown only to recover by looking for drivers to deliver to people in their homes, and to serve new B2B logistics needs. Lesson learned? The app-based ride service was resilient because its founder was decisive and creative, not solely because of technology.
Capria also found in analyzing its portfolio that an orientation toward investments in essential products and services to bottom-of-the-pyramid consumers, such as minorities, women, and refugees, has proven resilient because they serve critical needs even during times of uncertainty. Capria’s goals to “go beyond job creation and give low-income families access to goods and services that would otherwise not exist” has proven to be smart business in both good times and bad.

Susana Garcia-Robles (second from left) gathering with Co-Create LATAM.
Photo: Susana Garcia-Robles.
Other practices are pandemic-proof as well, such as their commitment to female fund managers and companies. Capria looks for women fund managers because as Garcia-Robles says, “[women] want to make just as much money as men, but…they also want to see if they can better the community and take care of the environment through their results and companies.” In fact, fund management teams with female managers invest in as much as 70% more female-led businesses compared to all-male teams. Capria also maps a company’s impact onto the Sustainable Development Goals (SDGs), creating “migrants to impact,” or companies that have begun to recognize their social impact when they consider their business’s contributions to the SDGs.
The long game
As the impact investing industry matures and Capria’s role in it continues, the tension—real or not—between social and financial gain will play out on an increasingly larger stage. We may be seeing, as Capria co-founder Will Poole said recently, “a cultural shift away from traditional notions of capitalism where profits trump all.” Time will certainly tell.
In the meantime, Susana and the Capria team are focused on ensuring that their funds, companies, and fund managers are around for the long haul. “Everyone has COVID fatigue but we really have to make sure our teams…are being creative and innovative and if you will, even energized by this. This has to be looked at as a new challenge, totally unexpected that the whole humanity is facing. And we’re going to come out better, knowing many new things.”
Back to Top
Goalmaker
Sasha Muench, Mercy Corps Country Director, Palestine
By Andie Long
 Sasha Muench, a twenty-year veteran of the international humanitarian and development agency Mercy Corps, had seen more of the world before she was a teenager than most people do in a lifetime.
Sasha Muench, a twenty-year veteran of the international humanitarian and development agency Mercy Corps, had seen more of the world before she was a teenager than most people do in a lifetime.
“For the formative years of my life, I was a nomad,” she says.
Both of Muench’s parents were development workers, trained in urban planning, and she and her sister grew up travelling across Africa and East Asia. She’s thankful her parents didn’t shield her and her sister from the realities of the places where they lived. “We did a lot of travelling, but always on a budget, very local. So I saw a lot of the world, and the grittiness of the world and the inequities.”
Together with their parents, she and her sister moved about every five years, a rhythm of life she continues to seek out today.
When Muench turned twelve, the family moved to the small town of Sequim in Washington state. “It was total culture shock,” she recalls. Muench knew that when she grew up, she wanted to return to the nomadic life.
‘Sometimes a loan isn’t enough’
As she was contemplating her future career, Muench said her father advised her: “‘don’t become an urban planner, it’s a useless degree. Go become an economist because they actually know how to solve problems.’ But then, “I became an economist,” she said, “and I thought, I’m not sure economists know how to solve problems either!”
The first major challenge in her career was supporting economic recovery after the war in Bosnia and Herzegovina. At the time, she says, there was a recognition that sometimes what people needed most was a loan to get back on their feet. As the work evolved, however, Muench and others came to see that often a loan wasn’t enough. In addition, she said, “you need connections, you need capacity, you need to know your markets.”
From there, Muench gravitated towards business development, and eventually she began working with institutions that could support individual business owners.
It was after the 2004 Indian Ocean earthquake and tsunami, when Muench was working in Indonesia, that she had an epiphany: “if we actually worked with the financial institutions to help the businesses recover, we could set up a long-term system that would help both of them.”
This thinking culminated in one of the most audacious programs of her career – the formation and launch of a wholesale microfinance bank in Indonesia. Together with a handful of socially-minded investors, including the Gates Foundation, Bank Andara was established to offer a range of banking products and services to hundreds of microfinance institutions, serving tens of thousands of retail clients in the island nation. Though Muench says Mercy Corps sold its share in the bank several years ago, Bank Andara continues to be one of the humanitarian agency’s top microfinance partners in the region.
‘Working ourselves out of a job’
As with Bank Andara, Muench approaches every humanitarian challenge with one thing in mind – sustainable change.
“I don’t want to be doing this work forever, and I don’t want to keep repeating the same things,” she says. “I think in the humanitarian industry as a whole, we should be working ourselves out of a job. And to do that we need to look at these broader systems.”
To do this, Muench leans heavily on her economics training. “What I like about markets in crisis,” she says, “is it’s using a lot of the principles around how economics works, and incentives, and how communities work, and applies it to moments of big change to see if we can lay the groundwork for long-term opportunity.”
“A chicken is not a job.”
While many development agencies tout gifts of livestock to poor families as a way to increase their incomes, particularly around the holiday season, Muench is known within Mercy Corps for her sassy retort – “a chicken is not a job!”
That said, Muench does think chickens are a great example of how taking a systems approach can create sustainable change.
“If you look at the poultry sector there are a lot of jobs, there are a lot of opportunities in there – from growing chickens, to processing them, to selling them, maintaining hygiene standards… If you actually work on that system, then it can create sustainable livelihoods for many people, and keep people alive, and healthy and fed. We shouldn’t be going around handing out chickens for the rest of our lives. We should be making the poultry system work so that people can live decent lives within that system.”
Muench insists there is an instinct in the industry to want to be the hero. But the more challenging and long-lasting approach, she says, is figuring out a way to help people solve their own problems.
“At the very least, because I am not here permanently, if I solve a problem, who’s going to solve it next time? So the best thing is if I can help somebody who’s going to be here forever, figure out the solution, and then they can keep adapting and changing so that people can get better. And if we don’t think about that, we can inadvertently do harm.”
Ultimately, it comes back to economics, she says. “When people are starving, we want to go in and give food. But then if we import a lot of food, what do we do with those farmers who suddenly can’t sell their crops because everybody’s got free food? Or the shopkeeper who can’t sell bread because everybody got free bread. But if we go and either give people cash so people can go buy the bread, or at least buy the bread from the shopkeeper and distribute it, then we’ve helped local business, we’ve helped people continue to maintain their business, and employ people, and helped the local economy grow.”
Opportunities in Palestine
Six months ago, Muench took a new position as Mercy Corps Country Director in Palestine, and moved to Jerusalem, along with her “cranky cat,” Izzy.
Though the role is one she admits she never anticipated wanting, she immediately found herself fascinated by the challenge. “There’s so much need here,” she says, “but it’s not a place that attracts a lot of philanthropy because of the politics.” That said, there is a great deal of opportunity: “If you look at the potential for economic growth in Palestine, it has a lot of the components it needs.”
One of the programs Mercy Corps runs in Palestine is Gaza Sky Geeks, a tech accelerator that supports entrepreneurial youth in earning a decent living through online freelancing and coding.
Not long after Muench arrived to take up her new role, COVID-19 hit. Most of the businesses Mercy Corps was working with in the West Bank had to close down, while the Gaza Sky Geeks continued operations, more or less as usual.
Mercy Corps currently has 50 staff in Palestine, most of whom are from the region. A majority are in Gaza, and the rest work in Jerusalem and Ramallah. Because of the technical savvy of the Gaza Sky Geeks staff and participants, they were able to shift to remote work fairly quickly, Muench said. They even managed to run a three-day online hackathon with 1,000 participants, called “Hack the Crisis Palestine,” which invited tech entrepreneurs to come up with solutions to the new COVID-19 reality. One group of entrepreneurs developed an app to support people’s mental health needs, enabling professionals to put their services online so people could find and use them.
What’s next?
Maybe it’s the COVID lockdown talking, but despite her nomadic ways, Muench has lately found herself hankering for the Pacific Northwest.
“I know this is probably really ironic for people stuck at home in Seattle and on the Peninsula, but as a Washingtonian who can’t come home right now, I want everybody to appreciate it,” she says. “All I want to do is go to the Dungeness River Center and stand on that bridge looking over the Dungeness River among the fir trees and look at the fish and just be home.”
Back to Top
From Our Blog
Responding to COVID-19 with Financial Inclusion Solutions
By Ed Cable, President
Mifos Initiative

A gathering of Mifos partners. Photo: Mifos
Governments everywhere are seeking to soften the blow to small and microbusinesses from the COVID-19 pandemic, and to provide transfer payments to the most vulnerable individuals. At Mifos, we’re intent on bringing open source technologies for financial inclusion to meet this moment.
Continue Reading
Responding to COVID-19 with Financial Inclusion Solutions
By Ed Cable, President
Mifos Initiative

A gathering of Mifos partners. Photo: Mifos
Governments everywhere are seeking to soften the blow to small and microbusinesses from the COVID-19 pandemic, and to provide transfer payments to the most vulnerable individuals. At Mifos, we’re intent on bringing open source technologies for financial inclusion to meet this moment.
Continue Reading
June 2020 Newsletter
Welcome to the June 2020 issue of the Global Washington newsletter.
IN THIS ISSUE
Letter from our Executive Director

Over the last few weeks, the U.S. has been gripped by unrest resulting from centuries of smoldering systemic racism that caught fire in the midst of a global pandemic. Global Washington stands with the Black Lives Matter movement and recognizes that Black communities in the U.S. are disproportionately impacted by COVID-19. As the disease continues to spread throughout the developing world, we see how those who are most marginalized by society are exponentially more vulnerable to health threats.
Global Washington members have been responding to the COVID-19 health crisis in many ways. Our members are also providing life-saving services for non-COVID-19 health issues that are critical for so many people around the world.
During the 2013-2016 Ebola crisis, in addition to all those who died from that swift and frightening disease, disruptions in routine medical services caused an estimated 10,000 preventable deaths from HIV/AIDS, malaria, and tuberculosis alone. As we take on this novel coronavirus that is sweeping the globe, we remember that the choice is never either, or – it is yes, and.
Despite the fact that COVID-19 is challenging us in ways we never imagined, children still need their regular vaccines. Pregnant women still need a safe place to deliver their babies. And cancer patients still need their medications.
Someday, we will better understand this virus – the ways it spreads, the ways it attacks the body, and the ways in which we can keep it in check. And in the meantime, we are seeing extraordinary ingenuity, borne out of necessity, to keep all of our other global health priorities on track. Many Global Washington members are doing just that. You can read more in this month’s issue, with special features on Fred Hutchinson Cancer Research Center and The Max Foundation.
The Pacific Northwest is known for our innovative global health organizations and our commitment to tackling difficult challenges. I find hope in the work of Global Washington members who are dedicated to saving lives and making the world a better place. I hope you do, too.
Kristen Dailey
Executive Director
Back to Top
Issue Brief
Navigating Global Health Priorities During a Pandemic
By Amber Cortes
Just a few short months ago (but what already seems like a lifetime ago), COVID-19 began to wreak havoc on the world. There’s been no sector left untouched by this pandemic—from work and economic growth to food security and education, and of course, global health.
COVID-19 and its economic consequences threaten to upend so much of the work that’s been done in the global health development community—and to stall progress towards the Sustainable Development Goals for 2030.
First, there are the immediate effects: disrupted supply chains, a squeeze on health system capacity and resources, confusion about health safety protocols, and lockdowns that prevent access to treatments and life-saving medicines.
The United Nations Children’s Fund (UNICEF) reported a 70% to 80% drop in vaccine shipments since March due to pandemic-related shipping and logistics challenges. Because of this, many preventable diseases like measles, polio and cholera are expected to rise. According to the Measles and Rubella Initiative, up to 117 million children worldwide could miss out on measles vaccinations since immunization campaigns were suspended to deal with the novel coronavirus.
Many organizations have had to shift their strategic goals for the year toward providing emergency response services, in many cases halting or significantly adjusting their regular programs and reconfiguring their supply chains in order to keep serving their populations, all while trying to navigate new realities, both known and unknown, of COVID-19.
But there’s even more at stake than that. COVID-19 has the potential to roll back decades of progress made in addressing many non-communicable diseases (NCDs). According to the Global Malaria Program, COVID-19 impacts could double the number of malaria deaths in sub-Saharan Africa from just two years ago. Another report by Stop TB Partnership projects an additional 1.4 million TB deaths during that same period. And a six-month interruption in the supply of anti-retroviral drugs (ARVs) could double AIDS-related deaths, essentially ‘setting the clock back’ to 2008 levels.
Then there are all the interruptions to regular and ongoing critical health services: for cancer patients who need chemotherapy, for example, or for women who need protection from gender-based violence or access to contraception and neonatal care.
When it has all been said and done, the COVID-19 crisis will have profound consequences for the world. The Global Washington community has stepped up in extraordinary ways to meet the immediate needs of this health crisis—and is working to build more resilient healthcare systems that are adaptable, scalable, and universal.
We know it’s a long road ahead, and that the complexity of the COVID-19 crisis has yet to be fully understood. There’s important, valuable work being done in all sectors right now. The following highlights some of the work being done by GlobalWA members.
Data-Informed Decision-Making
The Bill & Melinda Gates Foundation
The Bill & Melinda Gates Foundation is leveraging its twenty-years of experience in global health innovation to support vulnerable communities in African and South Asian countries. At home in the U.S., the foundation is focused on education-related needs, such as emergency aid to colleges to help mitigate closings, and developing online learning modules for K-12 students.
According the World Health Organization (WHO), Africa could become the next epicenter of the pandemic. There are severe shortages of both personnel and equipment, such as ventilators and personal protective equipment (PPE). A Reuters survey found that even in a best-case scenario, African countries would need at least 111,000 more intensive care beds and ventilators to meet the projected needs of patients. In response, the Bill & Melinda Gates Foundation is donating an additional $100 million to help prepare clinics to treat and isolate patients who may be infected with COVID-19, and to create protocols for contact tracing and infection control.
The Coalition for Epidemic Preparedness Innovations (CEPI), co-founded by the Gates Foundation in 2017, is helping scientists race for a vaccine with their COVID-19 Therapeutics Accelerator. In a bright spot of coronavirus news, the site reports that trials of potential treatments are already underway and the Gates Foundation says they will mass-produce any COVID-19 vaccine they develop to make it accessible and affordable.
Tableau Foundation
Software company Tableau’s free, publicly-accessible COVID-19 Data Resource Hub includes real-time data on case reports from Johns Hopkins University, the WHO and the CDC, as well as a curated gallery of visualizations from national news and health organizations.
The foundation has also ramped up its Community Grants Program, expanding the number of grantees and streamlining the application guidelines. Tableau has created two other giving campaigns for employees: one to support frontline health workers, and another, the COVID-19 Response Fund, to meet the needs of community organizations and non-profits serving at-risk communities that are disproportionately impacted by the disease and its repercussions.
Global Good
The Institute for Disease Modeling (IDM) is an institute within the Global Good Fund, a collaboration between Intellectual Ventures and Bill and Melinda Gates. IDM publishes models and studies disease transmission dynamics for malaria, polio, tuberculosis, HIV, pneumonia, typhoid, and more. Since COVID-19 struck, IDM has been instrumental in providing epidemiological models that predict transmission rates, collaborating with Fred Hutchinson Cancer Research Center, Microsoft AI for Health, and Washington State Department of Health officials to guide counties in Washington State towards an informed and safe re-opening.
Their comprehensive COVID-19 Infohub incorporates data on COVID-19 transmission rates along with economic impact projections in Washington State and around the world. It includes two powerful models: one for COVID-19 epidemic analysis, and a health systems model to help hospitals determine the number of ICU beds and waiting times needed for COVID-19 patients.
Fred Hutchinson Cancer Research Center
When COVID-19 first hit, the Hutch rallied its global teams of scientists and researchers who have experience tackling global health threats like AIDS and Zika. In addition to keeping those efforts on track, they are now working to track and assess the COVID-19 pandemic’s viral spread, developing diagnostic tests, and designing vaccines to prevent future outbreaks.
One way the Hutch is gaining insights into the virus is through a rapid genome sequencing tool called Nextstrain that builds viral “family trees” to track how and where the virus moves. It’s a “genetic jigsaw puzzle” that can provide clues to viral mutations in samples across the globe.
Keeping Non-Communicable Disease Targets on Track
PATH
People with underlying health conditions caused by non-communicable diseases (NCDs), whether cardiovascular disease, diabetes, respiratory diseases, or cancer are at higher risk for COVID-19 complications and death. Now, it’s even harder for these patients to get access to medications and diagnostic services—challenges that already existed before in many areas, but have been intensified by COVID-19.
During the Ebola outbreak in West Africa, health service disruptions caused 10,000 preventable deaths from HIV/AIDS, malaria, and tuberculosis. Citing the lessons from Ebola, PATH recognizes how crucial it is to protect the progress made on malaria prevention—which saves nearly 600,000 loves per year. As a result, they are adapting their delivery channels to continue bringing essential health services and important preventive measures like insecticide-treated bed nets to communities, while minimizing COVID-19 transmission.
In partnership with the WHO, Bill & Melinda Gates Foundation, Global Fund, PMI, and other organizations, PATH is also using data to detect new COVID-19 hotpots around the globe and modeling scenarios for how the virus may impact malaria transmission rates in high burden areas across Ghana, Kenya, and Malawi. PATH is also partnering with leaders in Senegal and the Democratic Republic of the Congo to integrate data visualization from information provided by national Emergency Operations Centers and National Malaria Control Programs.
By mapping out health priorities with real-time data and monitoring delays in drug manufacturing supply chains, PATH and its partners are able to build a sustainable tracking system that can respond to diseases long after COVID-19 is fully contained.
Malaria No More
“People all over the world now have an all-too personal experience with how a deadly, infectious disease can upend health systems and economies—and, more personally, how it can do the same to our families and communities,” says Martin Edlund, Chief Marketing Officer of Malaria No More.
Malaria deaths and cases were at their lowest levels ever recorded in 2018. Since then, progress has stalled, and now, COVID-19 could bring malaria back to 2000 levels—erasing the progress of the last twenty years. With the rainy season on its way in many parts of the world, Malaria No More has been intensifying its routine distributions of long-lasting insecticide-treated bed nets in the highest-burden villages.
“We have a critical window to support high-burden countries in taking actions that will save hundreds of thousands of lives and prevent health systems from being overwhelmed with tens of millions of additional malaria cases,” says Edlund.
Along with PATH, the Malaria Atlas Project, and the Bill & Melinda Gates Foundation, Malaria No More helped create a modeling analysis for the WHO with nine COVID-19 scenarios—and detailed what countries can do to save lives through early intervention efforts. The study found that India and many countries in Africa face a “dangerous double jeopardy” with peak transmission of both malaria and COVID-19 colliding in the next few months.
“The Ebola outbreak taught us that the best defense is a good offense,” says Edlund. Relying on data-driven decisions to stay ahead of both COVID-19 and malaria outbreaks will save lives. “By preventing, screening, diagnosing and treating malaria symptoms at the local level, countries can avert a devastating surge in severe-malaria cases at district and national hospitals.”
The Max Foundation
For The Max Foundation, COVID-19 has made it harder to fulfill their mission—getting crucial cancer medications across borders and into the hands of patients in low- to middle-income countries.
“In the case of The Max Foundation, our work in supply chains has been impacted in a number of ways directly as a result of COVID-19,” says Neal Parry, The Max Foundation’s senior supply chain manager.
There have been new restrictions on importing medicines, changes in cargo flight availability, and points of entry closures. But The Max Foundation is finding new solutions for home-delivery of medicines through local distribution partners, shifting from paper to digital prescriptions, and having physicians dispense a few months-worth of treatments ahead of time to last patients through the shutdowns.
“This pandemic has shown that there is no “one-size-fits-all” approach that will be successful in global supply chain operations,” Parry says. “However, it has shown that leveraging an organization’s network can create additional opportunities for collaboration.”
Burkitt’s Lymphoma Fund for Africa
Burkitt lymphoma (a form of non-Hodgkin’s lymphoma that’s highly curable with chemotherapy) is the leading cause of pediatric cancer deaths in equatorial Africa. Met with the sudden challenge of needing to procure personal protective equipment (PPE) for front-line healthcare workers, Burkitt’s Lymphoma Fund for Africa (BLFA) is now channeling immediate funds into procuring PPE in their grant network.
“In addition to sorely needing PPE, there are other situations that we are helping our grantees address (COVID-19) through this emergency fund,” says Karen Osofsky Michelson, a BLFA board member. They’ve helped one grantee in the network, a shelter in Tanzania where children and their families can stay during cancer treatment, to create an “isolation house” for quarantine purposes. They are also meeting transportation and meal costs for their patients and clinic employees.
“In essence, our fund provides a holistic, full life-cycle approach to keeping children safe and healthy. It goes way beyond the needs for PPE,” Osofsky Michelson says.
Meeting Healthcare Needs in a Crisis
Adara Development
A recent report released by the medical journal The Lancet modeled two COVID-19-related scenarios affecting some of the more vulnerable groups that Adara serves: pregnant women, and children. If maternal coverage and newborn interventions are reduced by 15% over the next 6 months due to COVID-19, there will be an almost ten percent increase in child deaths (under 5 years old) per month. If coverage reduces by 45%, the situation becomes even more dire: likely a 44.7% increase in mortality per month.
Adara is meeting the immediate needs of the COVID health crisis by delivering PPE, including thousands of N95 masks, to remote districts in Nepal, distributing soap to midwives in Uganda, and working on guidelines and protocols for staff in maternity and neonatal wards in both countries.
“Many of our programs are being adapted to respond to COVID-19 and its associated impacts. However, our goal is to maintain delivery of these critical health and education programs in order to help countries continue to drive toward the SDG targets,” says Brooke Magnusson, the global health partnerships manager (USA) for Adara.
Adara is shifting some of its educational programs, for example, by delivering curriculums through radio. And since the economic impacts of COVID-19 have affected food security, Adara has also been providing midday meals to children who can’t go to school right now.
Americares
Americares has a long history of disaster response, in particular to other outbreaks such as Ebola, Zika and measles. This experience makes the organization well-prepared to mobilize and distribute protective gear and infection control supplies that can help keep healthcare systems from becoming overwhelmed. Right now, Americares is mainly focused on maintaining capacity at under-resourced primary care clinics in Colombia and El Salvador. But Americares is also delivering masks (more than 2 million!), gowns, gloves and disinfectants to health facilities in 12 countries, and developing training modules on COVID-19 for healthcare workers.
Amplio
For Amplio, mobilizing communities is what they do best. The Amplio Talking Book is an audio device designed for low-literate adults and youth around the world to learn about such topics as malaria prevention, hygiene and sanitation. In response to COVID-19, Amplio is using its technology to link community media with district health experts and helping governments and media organizations align their key health messages to keep information consistent and credible.
PRONTO International
PRONTO International understands the language of urgency—the organization provides emergency training materials for health care providers in obstetrics and neonatal care. The organization was able to respond quickly to COVID-19 threats among its teams in Africa, India, and Central America.
For example, they’ve developed multiple COVID-related SIMPACs, or simulations—artificial scenarios where trained facilitators can use real-world events to educate others—to help teach providers to triage among COVID-19 obstetric patients and their babies. And for healthcare workers who are not trained as simulation facilitators, PRONTO International plans to release how-to videos and guidelines regarding COVID-19 management.
Spreeha Foundation
The Spreeha Foundation meets the challenge of poverty with a three-pronged, holistic approach—providing healthcare, education and skills training to underserved communities in Bangladesh. Now, COVID-19 has forced the foundation to temporarily close education and training services in order to ramp up its healthcare response.
“Overall, our SDG global health target has not changed,” says Ferdouse Oneza, CEO of Spreeha Foundation. “Although we are engaged in emergency responses, we’re keeping our long-term goals in focus. To that end, we are even pre-positioning ourselves with (a) more robust healthcare delivery system using telehealth.”
At the moment, Spreeha is working closely with the government of Bangladesh in providing health awareness messaging and door-to-door coronavirus screening services.
VillageReach
VillageReach solves health care delivery challenges in low-resource communities. When it comes to continuing its work amid COVID-19, “we need to be more creative than ever about how to do this,” says VillageReach President Emily Bancroft. This can mean using advanced technology—including deploying drones for delivery of medications or analyzing powerful datasets through OpenLMIS to forecast where medicines may be needed most during outbreaks.
The organization is also leaning into predictive analytics, such as in Mozambique, where VillageReach is collaborating with machine-learning firm Macro-Eyes to allow health workers to engage their communities. In Malawi, VillageReach has been collaborating with Global Good’s Institute for Disease Modeling (IDM) to predict COVID-19 transmission using datasets from sources like local health phones lines.
* * *
Besides the above highlights, check out our entire list of GlobalWA members who are working to improve health and healthcare in developing countries:
Back to Top
Organization Profile
Fred Hutchinson Cancer Research Center Expands World-Class Cancer Care in East Africa
By Andie Long

Kathleen Shannon-Dorcy (right), Fred Hutch nurse scientist & director of clinical/nursing Research, Education and Practice at Seattle Cancer Care Alliance, talks with an oncology nurse at the Uganda Cancer Institute. Photo courtesy of Fred Hutchinson Cancer Research Center.
When Fred Hutchinson Cancer Research Center (“the Hutch”) launched its partnership in 2008 with the Uganda Cancer Institute (UCI) in Kampala, Uganda, there was exactly one oncologist for the entire East African country of 43 million people. Today there are 14 clinical oncologists, and more are being trained every year.
While the oncologist is typically the individual in the white lab coat, the one everyone in the clinic looks to for definitive answers and direction, skilled oncology nurses are the people a cancer patient depends on most. They are the ones who know how to start and maintain an IV, administer the right drugs, check vital signs, alert the doctor to any significant changes, and in the case of UCI, arrange transportation for patients and their families to and from the clinic, a roundtrip journey that can be over 100 miles.
“The most important person on the care team is the nurse,” says Dr. Houston Warren, head of Global Oncology at the Hutch.
A researcher and practicing physician himself, Dr. Warren’s goal is to adapt the work that the Hutch is doing in Seattle for cancer patients all over the world. In order to do this, the Hutch Global Oncology team is finding ways to increase the number of people who can navigate the complicated world of cancer research, diagnosis, and care. Not just nurses and doctors, but also laboratory technicians, clinical coordinators, and more.
“Training providers at all levels is an important part of our mission,” he says.

Clinical staff from Fred Hutch, Seattle Cancer Care Alliance, and UCI pose in front of the UCI-Fred Hutch Cancer Center. Photo Credit: Mizan Howard, Fred Hutch Global Oncology Program.
Using Technology to Expand Human Capacity
Despite the urgency of training more Ugandan oncologists, nurses, clinical researchers and support staff, one human resource challenge that Warren believes can be transformed through technology is the role of the pathologist.
As it now stands, UCI staff can send digital microscope images of Ugandan patients’ tumors over the internet to a server in Seattle, where a Fred Hutch pathologist can review them the next morning and record her findings. Then every Wednesday at around 10pm Pacific Time, the Fred Hutch Global Oncology team in Seattle joins a virtual “tumor board” with their colleagues in Uganda to review the high-definition scans and the pathologist’s reports, look over patient histories, and discuss treatment options.
Pathologists, like other specialties, are in very short supply in Sub-Saharan Africa. At present there are fewer than 15 in all of Uganda, according to Warren. In addition to training more Ugandans pathologists, Warren sees potential in using artificial intelligence to amplify the work of each pathologist. Using high-throughput analysis, for example, could allow them to flag cases requiring priority review.
“Data science and AI have enormous potential for reducing global cancer disparities,” Warren says. Although the Hutch is not currently using artificial intelligence to help analyze pathology images from Uganda, this approach is part of Warren’s long-term vision for expanding the Global Oncology program.
In addition, new technologies may one day enable pathologists in Uganda to leapfrog current methods for tumor diagnosis and monitoring. One such approach is liquid biopsy, a technique that allows pathologists to identify molecular markers for cancer in a small sample of a patient’s blood. These highly sensitive tests would enable oncologists to identify and treat many more forms of cancer, especially those that can be difficult to biopsy and track over time.
Unique Needs of Cancer Patients in Uganda
Like many Sub-Saharan African countries, Uganda’s citizens are quite young. According to Warren, about 86% of Ugandans are under 40, and a third of the population is younger than 10 years old. Not surprisingly then, at UCI, many of the patients are kids.
There’s also a different mix of cancer types than the Hutch normally sees in Seattle. For instance, roughly a third of the cancers are infection-related – including Burkitt lymphoma, which is often associated with Epstein-Barr virus; Kaposi sarcomas that are associated with HIV; and cervical cancer, which can arise from certain types of persistent HPV infections. As far as non-infection related cancers, breast cancer is also on the rise in Uganda and across sub-Saharan Africa.
In addition, many of the cancer patients who visit the UCI frequently have underlying conditions that can make diagnosis and treatment a challenge. For example, in addition to the cancer, their bodies might also be grappling with malaria, tuberculosis, and various tropical infections, such as worms or other intestinal parasites.
Given these challenges, Warren says the Hutch is conducting clinical research to ensure that their interventions are “just as safe and effective as they are in Seattle.”
As a clinical researcher himself, Warren practices oncology at the Seattle Cancer Care Alliance once a week, and there is one question that drives him above all else.
“I have access to drugs that still aren’t available in Sub-Saharan Africa,” he says. “The drugs I use in my everyday practice are only available to at most 1 billion people or so, if that. And most of the cancer is obviously in the other 6.5 billion people. So how do we get those drugs, these unbelievably exciting and remarkable drugs that have been developed over the last 20 to 30 years, how do we get them to that majority of the population who could also benefit from them?”
The Impact of COVID-19 on Clinical Research and Treatment
The global COVID-19 pandemic has had a profound impact on the UCI since March, Warren said. Their research has been completely suspended in Kampala and only patients who are receiving direct treatment are able to visit the clinic.
“I’ve been surprised at the trajectory of the pandemic so far,” Warren said. “Most modelling of the disease for Sub-Saharan Africa suggests that cases will peak in July and August. Which makes it all the more reason to prepare as best we can and get more resources for testing.”
Even with the lockdown in Kampala, the Hutch and UCI have been building up their COVID-19 testing capabilities so that when cancer patients arrive for treatment they can be tested both to see if there is active infection from the novel coronavirus, and also to see whether they have been exposed to it at some point in the past.
“If we’re going to get our research program up and going again, we’ll need to have good COVID-19 testing going. It’s going to be a co-morbidity that will be important to be aware of long before this predicted peak.”
As far as how the pandemic will impact their global cancer work over the long-run, Warren says, “One possible scenario is that COVID-19 will become just one more potentially lethal infection that Uganda and the other countries in Sub-Saharan Africa have to deal with on a constant basis – added to malaria, TB, HIV, bacterial diseases, other viral diseases…” That said, he noted, “We don’t yet know what the impact [of COVID-19] will be on individuals living with HIV infection. That’s something we definitely need to study.”
High-impact, affordable diagnostic tools and therapies
Given many of the resource limitations in Uganda, the clinical researchers at the Hutch and UCI are studying ways to provide highly effective therapies to cancer patients at a lower cost. For instance, a breast cancer trial underway in Kampala is evaluating a combination of oral chemotherapy drugs for women who have locally advanced breast cancer. Since the COVID-19 pandemic got underway, patients in the clinical trial have been receiving a month’s worth of medications at a time – allowing them to bypass frequent clinic visits – a workaround that wouldn’t be possible with chemotherapy drugs that have to be delivered through infusions.
Another study is looking at a method of administering Rituximab, a targeted cancer therapy, under the skin (subcutaneously). If the approach is effective, it could replace the daylong infusions needed for that drug – a significant time-saver for patients and staff.
The Hutch currently has 30 clinical cancer trials underway in Uganda, investigating five different types of cancer and six associated viruses. In addition to its research center in Kampala, the Hutch also has a research center in Cape Town, South Africa, where the focus is primarily on developing a vaccine for HIV. While the Uganda lab focuses on cancer research and treatment, including a large focus on infection-related cancers, Warren hopes that one day the research activities of the two centers could be more deeply integrated. “There are lots of synergies possible,” he says.
Back to Top
Organization Profile
Building Bridges to Access: For The Max Foundation, Treatment is a Human Right
By Amber Cortes

Pat Garcia-Gonzalez, Chief Executive Officer of The Max Foundation, meets a local cancer patient and advocate in Ghana, 2018. Photo by Martin de Bruin.
According to Pat Garcia-Gonzalez, Chief Executive Officer of The Max Foundation, being told you or someone you love has cancer is one of the worst things that can happen in a person’s life—and she knows, because she went through it. Her stepson Max was diagnosed with chronic myeloid leukemia (CML) in 1988.
“But the only thing that’s worse than hearing that,” she adds, “is to be told that there is a treatment, but because of the place where you are—you cannot have it.”
It’s a frustrating reality of oncology many people aren’t aware of—the majority of new “revolutionary” cancer drugs that are discovered and come to the market aren’t even registered in most countries around the world.
“These drugs are made for the Western world,” Pat says. “In developing countries, often they’re just not available.”
For Garcia-Gonzalez, bringing life-saving drugs to patients in these countries is a moral obligation, “and it’s the responsibility of drug manufacturers to develop global access strategies, and of governments to participate in bringing these drugs to the patients.”
“We believe that access to treatment is a human right,” she added, “and there is no reason in my mind why people should die because they don’t have access to these treatments.”
Tragically, Max passed away in 1991— “a very genuinely loving kid, whose life was robbed too young, you know, he was diagnosed when he was 14, just a teenager,” says Garcia Gonzalez.
“Some people, when they go through what we went through, I think you have two types of reactions. One is to never want to hear the word ‘cancer’ again. And then I think there are people that refuse to accept that is the end, that it’s over. And there was this feeling that there has to be something more—it cannot be that Max passed away, and then you just go back to your life.”
Seeking to create meaning from this tragic loss, she started The Max Foundation in 1997 as a grassroots effort—a group email list, created to help support other parents of children with leukemia. Originally from Argentina, Garcia-Gonzalez expected to get only requests from parents of children from Latin America with leukemia.
“But to our surprise, from day one, we started receiving desperate emails from people all over the world, in a very similar situation, where they or their loved one had been diagnosed with some cancer, not just leukemia. They were told they needed a treatment, but the treatment was not available in their country.”
The Max Foundation’s mission is different than other cancer organizations—instead of focusing on finding a cure, they partner with pharmaceutical companies, hospitals, and oncologists to get life-saving medications and treatments that already exist directly to patients. To do this, they’ve built a sophisticated supply chain that moves medicine from just three warehouses to over 90 hospitals and clinics around the world.
The Max Foundation’s model—possibly the only of its kind in the world—works differently than typical humanitarian medicine donation models. They don’t just donate medicine for relief efforts; they seek to fill in the gaps of cancer care by operating as a bridge between resources and patients while improving supply chains and working with governments and distributors to get medicines approved and into the hands of patients.
And, as Garcia-Gonzalez learned, the challenges of building these bridges—securing donated medicine, or understanding shipping logistics, for example—are complex.
“Distributing medicines internationally is not for the faint of heart!” she exclaims.
In May 2001, Swiss pharmaceutical company Novartis released a groundbreaking, targeted medication called Glivec® (Gleevec) that transformed chronic myeloid leukemia treatment—turning a previously fatal disease into a manageable one.
And their new partnership forged with the company became a game-changer for The Max Foundation, as well—allowing them to serve more patients on a scale that they never thought possible.
“So here we were, you know, a small grassroots volunteer organization that now had the opportunity to help thousands of people—to fulfill our mission 100 times more,” explains Garcia-Gonzalez.
Together with Novartis, The Max Foundation co-developed a direct-to-patient international medicine donation model. The program proved successful—reaching more than 70,000 patients in almost 80 countries for 15 years.
Eventually, The Max Foundation leveraged what it learned from this partnership and developed its own program, called Max Access Solutions. Max Access Solutions is a unique treatment access model that prioritizes individual patients’ needs with the sophistication and flexibility to fit local regulations. Just last month, Max Access Solutions passed an important milestone—distributing over 10 million daily doses to patients in over 70 countries since the program’s inception in 2017.
But The Max Foundation’s role doesn’t just end once the patient gets their medication. Many patients need supportive care, as well, and The Max Foundation’s global on-the-ground team supports these patients by providing local patient services.
“So, for us,” Garcia-Gonzalez explains, “we literally put the patient at the center and then we think what is the best, most holistic approach to everything the patient needs? And let’s provide all those pieces, you know, from the access to treatment and diagnostics, to the emotional support that cancer patients and their families need.”
One huge piece of the puzzle of making patient-centered care more accessible in underserved countries is meeting the cost of diagnostics. CML patients have to be diagnosed and tested every three to four months to find out which drugs are most appropriate to their treatment and monitor their response to the treatment. Often the high cost of these tests remains a roadblock. On a 2009 trip to Africa, Garcia-Gonzalez discovered that cancer patients in Ethiopia were selling their homes just to cover the $600 for their blood tests, which had to be shipped to Europe for analysis.
“Those who could were selling everything they had to send their blood to Europe to get a diagnostic test,” Garcia-Gonzalez explains.
“And this is one of those things where I thought, ‘this is not possible. It just cannot be.’ So, when I came back, everybody I met, I told them this story.”
One of the people she told the story to was Dr. Jerry Radich, an oncologist at Fred Hutchinson Cancer Research Center, who specializes in the molecular genetics of leukemia. Radich connected her to Cepheid, a molecular diagnostics company that was developing a cheaper point-of-care technology with a CML specific kit. The Max Foundation entered into a preferential pricing partnership with Cepheid which reduced diagnostic testing costs from $600 down to $50.
Further, Dr. Radich later develop a cheap, affordable way to ship blood samples called “Spot On CML.” The patient puts a dried blood sample on a card that can be mailed to the Hutch for testing.
This award-winning solution, Spot On CML, is a stopgap—eventually The Max Foundation and the Hutch hope to provide high-end equipment to handle diagnostics onsite around the world. And since $50 is still a lot of money for many people, they’ve formed a Solidarity Fund so that more stakeholders can commit to making diagnostics affordable in the long run. Working with the world we have now is a big part of The Max Foundation’s philosophy.
And of course, the world we have now has been changed forever by COVID-19. The effects of the pandemic have been felt in every development sector, including and especially global health.
“I think I would be lying if I told you that COVID-19 is not impacting cancer organizations,” Garcia-Gonzalez says. “It is kind of bringing us back a little bit. So, we have to really reverse courses in a little bit of an unexpected way.”
For The Max Foundation, this has meant navigating around disrupted supply chains and cancelled appointments, as public hospitals become converted into COVID-19 clinics and medical supplies get re-routed. Still, Garcia-Gonzalez sees these problems as opportunities to make healthcare more responsive, adaptive, and resilient.
“I think that we’re finding some opportunities of things we could do better,” she says. This includes arranging home delivery of medications through drones, and using electronic prescriptions instead of paper, so the patient does not need to leave their home.
“And, you know, I’m hoping once we go back to normal, the new normal will include some of the lessons learned from COVID-19.”
Like others in the global development community, The Max Foundation is racing to meet the UN’s Sustainable Development Goals by 2030. It’s a daunting path ahead—while SDG 3 seeks to reduce non-communicable diseases (NCDs), like cancer, diabetes, and cardiovascular disease by one-third, the World Health Organization predicts that by 2030 the number of new cancer patients diagnosed each year will double worldwide, with the vast majority of those people—7 out of 10—living in underserved countries.
Despite the disruptions from COVID-19, Garcia-Gonzalez remains optimistic about meeting this goal. In part because she knows that one day there will be a cure, but for now—there are lives to be saved.
“I feel sometimes people assume that, ‘Oh, well, we cannot provide access to treatment because first we have to spend 20 years strengthening healthcare systems.’ And I want to challenge that assumption,” says Garcia-Gonzalez.
“What we have shown through the years is that by bringing these medicines, we strengthen the healthcare system, because we provide physicians with a way to safely and successfully treat cancer.”
Back to Top
Welcome New Members
Please welcome our newest Global Washington members. Take a moment to familiarize yourself with their work and consider opportunities for support and collaboration!
ChildFund International
ChildFund International promotes children’s development at each stage of life to ensure infants and young children are healthy and secure, children are educated and confident and youth are skilled and involved in their communities. ChildFund reaches over 10.5 million people across 24 countries – including the United States – through work with local partner organizations, governments, corporations and individuals. The organization works to strengthen child protection-focused institutions and policies by combining its programs with efforts to influence local and national leaders to prioritize the protection and well-being of children and youth. Approximately 200,000 Americans support ChildFund’s work through sponsoring individual children and investing in its programs. https://www.childfund.org/
Covenant House International
Covenant House International is the largest charity in the Americas serving and advocating for youth facing homelessness and trafficking. It offers a continuum of care to help young people move from poverty to opportunity and from homelessness to hope through shelter, education, job training, medical care, substance-use treatment, parenting support, and legal aid in 31 cities and 6 countries: Guatemala, Honduras, Mexico, Nicaragua, Canada, and the U.S. https://www.covenanthouse.org/
Back to Top
Member Events
June 15: Global Leadership Forum virtual info session for senior-level executive leaders
June 18: OutRight: COVID-19 and domestic violence
June 18: PATH: Building resilience during response – is it possible?
June 18: Seattle DE&I Community of Practice virtual day of learning
June 25: Outright: COVID-19 and national human rights institutions
Back to Top
Career Center
Executive Director/Senior Director of Development, Pilgrim Africa
Senior Accountant, VillageReach
Partnerships Director, Amplio
Consultant, Gorman Consulting
Check out the GlobalWA Job Board for the latest openings.
Back to Top
Future of Fish Helps Peru’s Small-Scale Fisheries Acquire PPE to Stay Afloat in Pandemic
By Julie Budkowski, Operations Director, Future of Fish

Pedro, a fisherman and youth leader in La Islila, Peru, carries boxes of donated soap to support the health of his fellow fishermen. Photo credit: Future of Fish.
Fishers are essential workers, but what happens when they don’t have the gear they need to work safely in a pandemic?
In Peru, small-scale fisheries play a critical role in food security, supplying approximately 95% of the seafood consumed domestically. But without personal protective equipment (PPE), even essential work such as fishing becomes too high risk, leaving communities without food or fishers risking their own health or livelihood. Sourcing the PPE and sanitation resources needed for businesses to open safely has been difficult in the developed world, and even harder in countries like Peru, where it is urgently needed and for many small-scale fishers and market vendors, nearly impossible to find.
The need for PPE is especially acute in Peru’s small fishing villages like La Islilla, where limited medical infrastructure, dirt road access and no running water means that the spread of COVID-19 would be catastrophic. La Islila is a small town on Peru’s north coast that was settled by fishermen back in the 1800s. It is a tight-knit community of 300 fishing families who use traditional fishing techniques to supply fish for both domestic and international markets.
Continue Reading




 Mark Dasco says that growing up in a poor family in a “far-flung village” in the Philippines taught him first-hand the realities of deprivation, exclusion, and vulnerabilities, but it also showed him just how resilient children and communities can be. But just because they are resilient doesn’t mean they should have to be.
Mark Dasco says that growing up in a poor family in a “far-flung village” in the Philippines taught him first-hand the realities of deprivation, exclusion, and vulnerabilities, but it also showed him just how resilient children and communities can be. But just because they are resilient doesn’t mean they should have to be.

 I have two children in Seattle Public Schools, so like many families across the U.S., I am filled with mixed emotions about online learning, rather than in-person classrooms. However, I am grateful that we have an online option and that the school district is working to donate computers to students who need them. For most children in low- and middle-income countries, online learning via computer is not a viable solution. Fortunately, several Global Washington members are working with local governments and schools to come up with creative alternatives, such as delivering educational curriculum to cell phones, as well as using radio and TV broadcasting.
I have two children in Seattle Public Schools, so like many families across the U.S., I am filled with mixed emotions about online learning, rather than in-person classrooms. However, I am grateful that we have an online option and that the school district is working to donate computers to students who need them. For most children in low- and middle-income countries, online learning via computer is not a viable solution. Fortunately, several Global Washington members are working with local governments and schools to come up with creative alternatives, such as delivering educational curriculum to cell phones, as well as using radio and TV broadcasting.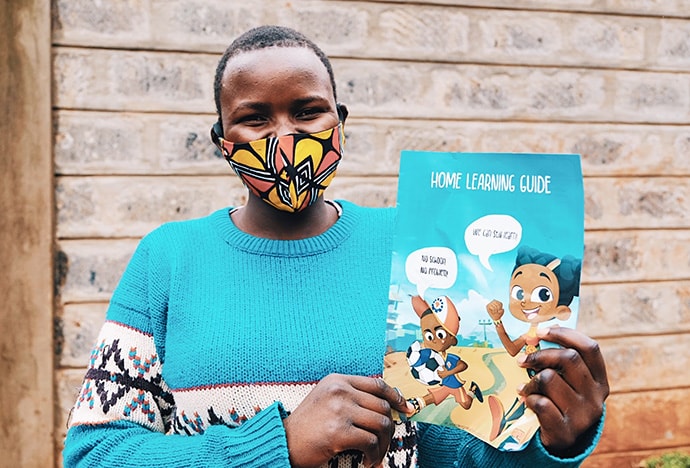




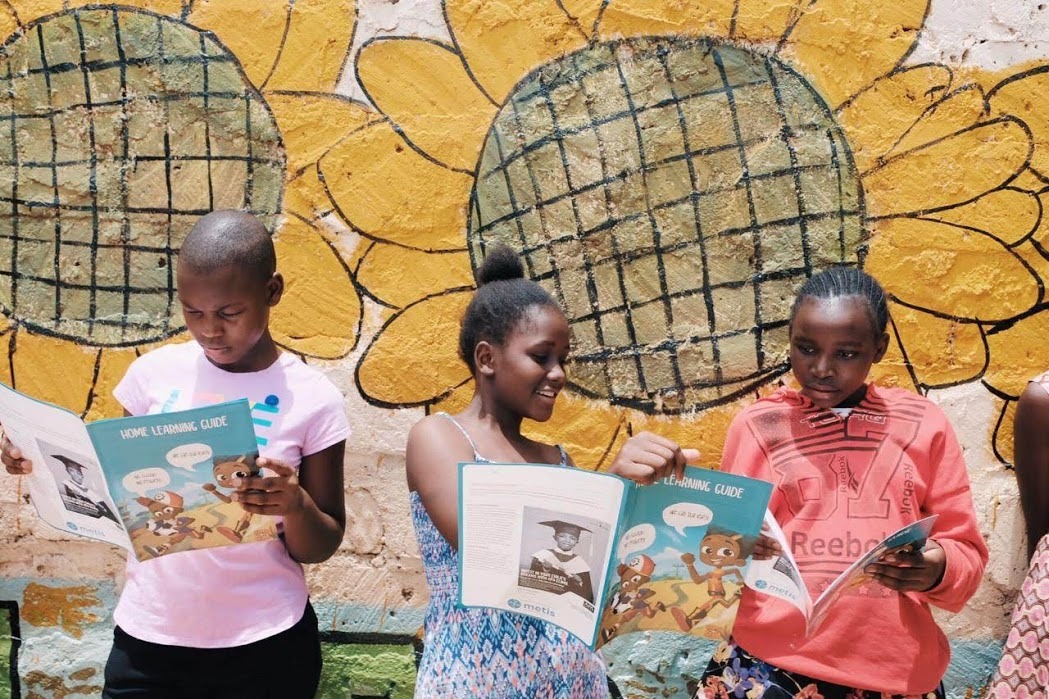






 Sasha Muench, a twenty-year veteran of the international humanitarian and development agency Mercy Corps, had seen more of the world before she was a teenager than most people do in a lifetime.
Sasha Muench, a twenty-year veteran of the international humanitarian and development agency Mercy Corps, had seen more of the world before she was a teenager than most people do in a lifetime.




