Recent Crises have Forced a Greater Awareness of the Need for Mental Health Programs
By Joanne Lu
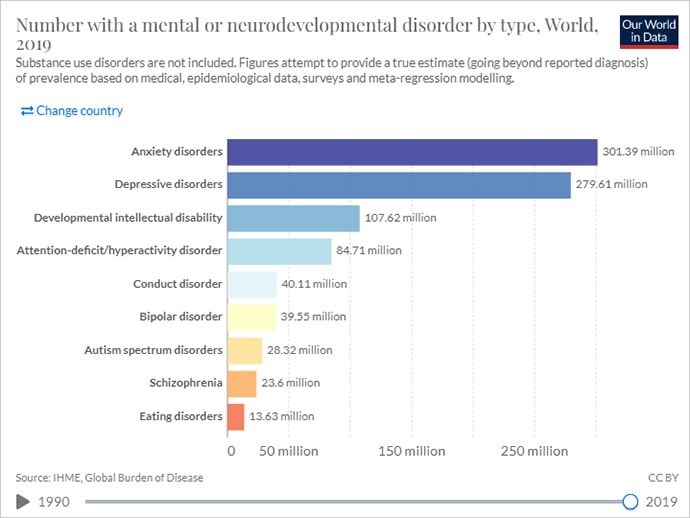
World mental disorders by type 2019. Screenshot of Our World in Data website.
We all feel the stress of the times in which we live in. But for people living in situations of economic insecurity, conflict, natural disasters, food insecurity, political instability, or daily human rights abuses – conditions that take an immense toll on a person and community – mental health often goes unaddressed.
Even before COVID-19 entered the world stage, mental and addictive disorders affected more than 1 billion people globally. But, according to the World Health Organization (WHO), in low- and middle-income countries, 75 percent of people with mental health conditions receive no treatment.
There are many reasons for this, says the global health organization PATH – one being stigma, which discourages people from seeking diagnoses and care. To bypass stigma, PATH is integrating mental health screening and services into already established routine medical visits. For example, in Mozambique, PATH collaborated with the Maternal and Mental Health Departments at the Ministry of Health to develop a protocol within routine postnatal care to screen and care for women with postpartum depression. They’ve also incorporated mental health care into existing HIV services in Vietnam and Kenya. By integrating mental health questions and conversations into routine visits, PATH says it becomes less about specific mental health issues and more about holistic care.
Low- and middle-income countries often also face a shortage of health-care workers. Even where there are enough health workers, lack of access to mental health care training is often an obstacle, according to PATH. This leads to low detection rates and a low prioritization of mental conditions. That’s why Americares not only deploys mental health experts to provide psychological first aid to survivors of disasters and emergencies, but they also train health workers to recognize and refer patients who need mental health support.
With low prioritization of mental health also comes lack of funding to sustainably scale proven interventions and service delivery models. In fact, less than 1 percent of health-related global development assistance has ever gone to mental health, according to several studies.
Last year, World Vision helped Congress introduce the Mental Health in International Development and Humanitarian Settings Act (or MINDS Act). It is the “first-ever U.S. legislation that addresses mental health and psychosocial support in foreign assistance,” said Margaret Schuler, World Vision U.S.’s Senior Vice President of International Programs.
The bill aims to codify the position of USAID Coordinator for Mental Health and Psychosocial Support. It will also require the integration of mental health and psychosocial support into U.S. foreign aid as well as USAID and State Department regional bureaus and missions. And the Executive Branch will be required to brief Congress on how implementation of the bill is going, the barriers to mental health and psychosocial support programming, and overall spending on mental health programming in U.S. foreign assistance. All these efforts will help maintain focus on the mental health needs of vulnerable populations, promote best practices, and lay the groundwork for a global mental health strategy.
In addition to advocating for more U.S. support on this issue, World Vision implements a range of mental health and psychosocial support programs in nearly 70 countries. World Vision is particularly concerned about the mental wellbeing of the world’s 426 million children who are living in conflict-affected areas as traumatic events can have lasting negative effects on children, even changing their genetic makeup and passing those changes onto the next generation. Hormones released during times of heightened stress can lead to other negative health consequences as well. According to World Vision, more than 1 in 5 people living in conflict-affected areas have a mental health disorder.

Afghani child. Photo: ArmyAmber, Pixabay
Similarly, mental health and psychosocial support is a core program priority for Save the Children. In Ukraine, for example, Save the Children has been working with a local partner, Slavic Heart since 2015 to deliver essential items to families and ensure children are protected and have access to mental health support. Right now, amid the Russian invasion of Ukraine, Save the Children is providing online mental health sessions for children through Slavic Heart.
Over the last two years, the pandemic has also exacerbated global mental health needs due to COVID-related grief, stress, anxiety, depression, and substance abuse. But according to a recent WHO survey, it has also interrupted or halted existing mental health care services in 93 percent of countries around the world. Health care workers and community health workers have been hit especially hard with depression, anxiety, insomnia, distress, and burnout, which in turn affects the quality of care they provide.

Healthcare professional, Angola. Photo: Francisco Venancio, Unsplash.
To help clinical educators who are training nurses and midwives become more conscientious teachers and clinical providers, PRONTO International built a virtual superhero comic that teaches clinical educators how to practice empathy, conduct self-checks for stress, and use other self-wellness tools that can be used throughout a busy day. This idea that checking in on one’s own mental health is a critical part of providing quality care is a “significant leap in global health,” says PRONTO. “More than just clinical skills are required for care to be respectful and high quality.”
Severe gaps continue to exist in mental health care, particularly in the communities that need it most. But organizations like these are working hard to help health-care providers and policymakers see how caring for mental health is a crucial part of caring for the whole person. Physical health problems can harm mental health, and vice-versa. Similarly, unaddressed mental health conditions can hold back progress on other SDGs, just as lack of progress on issues like poverty, hunger, and gender equality can cause mental distress.

“World Mental Health Day Observance” by United Nations Photo is marked with CC BY-NC-ND 2.0.
Especially amid protracted conflicts, climate disasters and the many lingering impacts of COVID-19, mental health support couldn’t come sooner for most of the world.
The following GlobalWA members are providing mental health services and programs in low- and middle-income countries.
Americares: Mental health is an important focus for Americares global health work, in our ongoing programs and responses to disasters and emergencies. Americares long-term goal is that everyone affected by poverty or disaster has equitable access to quality mental health services and programs. As part of our Emergency Programs, Americares deploys mental health experts to provide psychological first aid and other immediate support for survivors as well as help build local capacity for mental health services. To strengthen local health systems, Americares provides our health partners with training so health workers can recognize and refer patients who need mental health support. This includes programs to decrease stigma and discrimination, particularly in countries with the largest treatment gaps. Americares also provides behavioral medication to partners through our Medicine Security program. Many of Americares projects and programs incorporate mental health and psychosocial care – from programs focused on reproductive health to those that address chronic disease and disaster preparedness. In this way, Americares achieves its mission to save lives and improve health for people affected by poverty and disaster, so they reach their full potential.
Amplio: Strengthening Mental Health Education in Ghana’s Rural Districts: After the Mental Health Act 846 passed in 2012, Ghana Health Service (GHS) shifted its mental health programming from facility-based to a more community-based approach. GHS set up new structures, with regional, district, and facility-level mental health coordinators. But in the Upper West Region’s rural districts, the coordinators lack access to reliable training and support.
Too often, mental health education is left to community health workers who have no formal mental health training. Although GHS established self-help groups, only about 30 groups are active in the region, which has a population of over 900,000 people.
Amplio is working with GHS and UNICEF to improve access to mental health education as part of an ongoing public health initiative. Community health nurses and volunteers use Amplio Talking Book to share consistent health messages. Mental health topics include awareness, prevention, and treatment of maternal depression, domestic violence, and drug and substance abuse.
People can use the Talking Book to record questions and experiences that they might not share in a group setting. Talking Book user feedback is anonymous — unless someone chooses to identify themself. However, the data for each device is linked to a specific group or community, allowing us to address local issues and concerns.
Days for Girls: At Days for Girls, we work to eliminate the stigma and limitations associated with menstruation so that women and girls have improved health, education, and livelihoods. Lack of supportive menstrual health impacts a range of SDG outcomes including Goals 4, 5, 6, 8, 12, and 3 – including stigmatization and isolation that contributes to anxiety, depression, and in some cases even suicide. DfG recognizes the connection between dignified, supportive menstrual health environments and mental wellbeing. Our programs work to cultivate those safe spaces at the level of individual menstruators, families, and communities. At the grassroots level, DfG Social Entrepreneurs are also advocates and certified educators, leading conversations within their communities to break down stigma. At the international level, our Advocacy Program has worked to demonstrate the linkages between menstrual health and mental wellbeing, including our event for Self-Care Trailblazer Group’s 2021 Learning and Discovery series, The Role of Supportive Self-Care Environments in Advancing Menstrual Equity.
Fred Hutchinson Cancer Research Center: At Fred Hutchinson Cancer Research Center, interdisciplinary teams of scientists seek new and innovative ways to prevent, diagnose and treat cancer, HIV/AIDS and other life-threatening diseases.
Financial hardship after cancer diagnosis is unfortunately a common occurrence for people with cancer and their families. Financial hardship can be material, such as going into debt to pay for healthcare or having bills go to collections because of reduced employment during treatment. Financial hardship can also be psychological and emotional in the form of worry and anxiety about paying for healthcare and basic needs like housing and food.
Research from Dr. Salene Jones at Fred Hutch and others has shown that financial hardship leads to worse mental health and quality of life after cancer diagnosis. Dr. Jones is currently leading a study that will develop new tools to screen for financial hardship associated with worse mental health in people with breast cancer. These tools will include assessments for both material and psychological financial hardship and will help clinics address economic burden that leads to poor mental health outcomes such as depression and anxiety. This study will also examine potential employment policies that could reduce financial hardship after cancer diagnosis.
PATH: With programs in over 70 countries, PATH has witnessed the unmet mental health needs in the communities where we work. We also know that reduced access to mental health care services impacts health-seeking behavior or adherence to care regimens for other health conditions (e.g., diabetes, tuberculosis, HIV), leading to poorer health outcomes. As such, PATH has prioritized integrating elements of mental health care into existing programs at the primary health care (PHC) level.
Project examples include:
- HIV services (Vietnam): We incorporated mental health care into existing HIV services. In partnership with peer outreach workers and trained service providers, individuals are screened for depression, anxiety, addiction, and suicide risk and provided individualized care plans.
- Services for youth (India): We are co-creating an appropriate, accessible, and safe digital approach to support youth mental health care in partnership with young people.
- Postpartum depression/maternal health (Mozambique): We developed a novel protocol for the screening and management of women with postpartum depression within routine postnatal care alongside the Maternal and Mental Health Departments at the Ministry of Health.
Through these projects, as well as others underway, PATH sees the value of integrating mental health care services in the PHC setting and aims to expand this important work as a way to close the treatment gap for mental health disorders.
PRONTO International: We have built a virtual superhero comic with modules that help clinical educators (who are training nurses and midwives) to practice empathy, self-checks for stress and other self wellness tools that we believe will help them be more conscientious teachers and clinical providers. This targets the mental health of the clinical provider with simple tools that can be used throughout a busy day. This particular project is extremely innovative due to the virtual self-paced aspect, using a dynamic super hero comic to provide learning modules, and the focus on making it not only ok, but critical to check oneself and one’s mental space as part of providing quality care. This thinking represents a significant leap in global health – the emphasis that more than just clinical skills are required for care to be respectful and high quality. (PRONTO is the intervention with support from UCSF, University of Utah, and funding from BMGF)
Save the Children: Mental Health and Psychosocial Support (MHPSS) is a core technical programming priority for Save the Children. Within our Health, Education, and Child Protection work, MHPSS ensures that the mental health and psychosocial well-being of children and families is supported through multiple spaces including clinic, school, or center-based services, as well as through community and home support mechanisms.
One of Save the Children’s signature programs for providing structured psychosocial support to children, youth, parents, and caregivers is HEART (Healing and Education through the Arts), which is currently celebrating its 10 year anniversary. HEART uses expressive arts activities (art making and group discussion) to help children and adults to understand and express feelings, ideas, and experiences in an emotionally supportive environment. It supports stress processing and recovery and helps children and adults to develop skills to support themselves and each other in times of stress. To date, HEART has supported more than 1 million children in 30 countries around the world. To learn more, visit our website.
World Vision: World Vision implements a range of Mental Health and Psychosocial Support (MHPSS) programmes in all parts of the world, during emergency responses and also in development contexts. One of World Vision’s earliest programs in MHPSS was to develop a tool for measuring depression within the post-conflict Rwanda context. Using this tool, a series of Interpersonal Psychotherapy for Groups (IPTG) programmes were developed and later implemented in Uganda, particularly amongst people impacted by HIV/AIDS, with impressive results for sustained symptom reduction. As part of World Vision’s global strategy Our Promise we focus on a community-based MHPSS approach that:
- Ensures emergency responses are safe, dignified, participatory, community-owned and socially and culturally acceptable
- Maintains the protection and well-being of people in distress by strengthening community and family support
- Ensures that people distressed by mental health and psychosocial problems have access to appropriate care
- Ensures that people suffering from moderate or severe mental disorders have access to essential mental health services and to social care
- Ensure MHPSS activities are integrated into wider systems to advance the reach and sustainability of interventions and reduce stigma of stand-alone interventions, and
Strives to be integrated whilst building on existing capacities and upholding cultural norms.